This ECG was recorded at 25mm/s from a 72 year old male who was complaining of a prolonged period of chest pain at rest. He has a history of diabetes and hypertension.
How should the ECG be interpreted?
Dr Dave Richley,
Associate Lecturer
Newcastle University
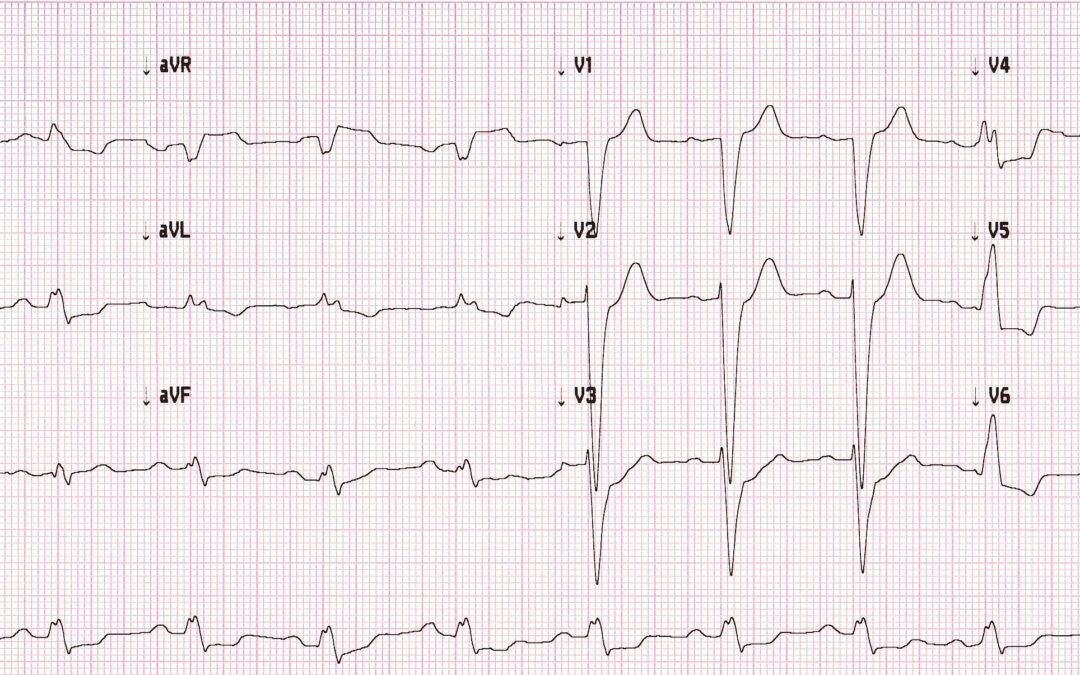
Sinus rhythm , normal axis, with wide QRS in LBBB morphology, concordant ST depression in V3 ( in lbbb)ST elevation in aVR with ST Depression in multiple leads. Indicative of A C S , Indicating LAD involvement, adv cath lab activation ……
St elevation in avr and v1 Concordant st depression in v2 and v3. There is st depression in more than 6 leads. Given the history and ecg changes, this signifies proximal lad occlusion. (Lad occlusion proximal to the 1st septal branch)
Sinus rhythm with LBBB and ST changes which would have to be reviewed in the clinical context.
Purely based on the ECG there is concordant ST depression from V2-V4 up to 4mm. Same but more subtle pattern on lateral leads. Would not rule out posterior/lateral MI
Hi Dave. Sinus rhythm with left bundle branch block. You could say there is appropriate discordance in leads I and V6, but there is ST depression in leads II, aVF, V3 and V4 (leads where you would probably expect the ST/T waves to be positive in LBBB). There is also ST depression in lead V5 – more than perhaps would be expected for LBBB. I’m just basing this all on pattern recognition having seen loads of LBBB under normal circumstances. In context of the history, I think then this is suspicious for ACS. Whether it’s post infarction or unstable angina – I don’t know. I also couldn’t guess what region/artery is involved. It doesn’t reach the criteria for Sgarbossa (or modified), as far as I understand it, so I’m assuming it’s not acute, but my reading on the subject is poor so I’m looking forward to the answer! As always, a previous ECG is helpful in these situations. Many thanks.
Thanks, Francisco and Max, for your comments. I won’t say anything at this point because I’d be interested to see other opinions first. Just one question though, Max – are sure this ECG doesn’t meet any Sgarbossa criteria?
Ok – is V3 what I missed in the criteria?
You might be on to something there! I’ll do a detailed response next week after I’ve allowed a bit more time for people to offer their own opinions first.
For many years it was believed, and to some extent it still is, that an acute myocardial infarction (MI) cannot be diagnosed from an ECG if there is left bundle branch block (LBBB). This is because LBBB, even in the absence of MI, causes ST elevation, Q waves and T wave inversion – ECG features that are normally associated with MI. For this reason, it has often been advocated that acute chest pain with new LBBB simply be regarded as a possible MI and the patient managed accordingly, although in practice it is often impossible to say whether the LBBB is new because no previous ECG is available for comparison.
However, a landmark paper published in 1996 (1) showed that is possible to diagnose or exclude MI from the ECG with a high degree of accuracy even when LBBB is present. The three Sgarbossa criteria, as they became known after the paper’s lead author, suggesting acute MI are:
• ST elevation ≥ 1 mm with a positive QRS
• ST depression ≥ 1 mm in V1, V2 or V3
• ST elevation ≥ 5 mm with a negative QRS
The more of these criteria that are satisfied, the greater is the likelihood of MI.
Let us now consider this month’s ECG in relation to these criteria. The ECG clearly shows LBBB, but instead of ST elevation in V1 to V3, as would normally be seen with LBBB, there is ST depression in V2 and V3. This fulfils the 2nd Sgarbossa criterion and, according to the 1996 study, this sign alone has a sensitivity of 78% and a specificity of 90% for acute MI. It is therefore highly likely that our patient, suffering from prolonged chest pain at rest, is having an MI.
Subsequent research has refined and added to the original Sgarbossa criteria to increase the accuracy of the ECG in diagnosing MI in the presence of LBBB. Smith et al found that the sensitivity of the 3rd Sgarbossa criterion could be increased by requiring ST elevation that is at least 25% of the amplitude of the Q or S wave, rather than a fixed value of 5 mm, in any lead (2). By this Smith modification, aVR in this case is positive for acute MI because there is 1.5 mm ST elevation and a QRS depth of 2.5 mm.
Most recently, in 2020, additional diagnostic criteria for acute MI in the presence of LBBB were reported in a study by Di Marco et al (3). One of the criteria extended the scope of the 2nd Sgarbossa criterion to a requirement for ST depression in any lead with a predominantly negative QRS rather than only V1, V2 or V3. By this criterion, V4 would additionally be positive for acute MI.
There is therefore ample evidence that this ECG, in the presence of prolonged chest pain at rest, is indicative of an acute MI.
References:
1. Sgarbossa, EB, Pinski, SL, Barbagelata, A, Underwood DA, Gates KB, Topol EJ et al Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle branch block. N Engl J Med. 1996 Feb 22;334:481-7. DOI: 10.1056/NEJM199602223340801
2. Smith SW, Dodd KW, Henry TD, Dvorak DM, Pearce LA. Diagnosis of ST elevation myocardial infarction in the presence of left bundle branch block with the ST elevation to S-wave ratio in a modified Sgarbossa rule. Ann Emerg Med. 2012 Dec;60(6):766–776. DOI: 10.1016/j.annemergmed.2012.07.119
3. Di Marco A, Rodriguez M, Cinca J, Bayes-Genis A, Ortiz-Perez JT, Ariza-Solé A, Sanchez-Salado JC, Sionis A, Rodriguez J, Toledano B, et al. New electrocardiographic algorithm for the diagnosis of acute myocardial infarction in patients with left bundle branch block. J Am Heart Assoc. 2020 Jul 21;9:e015573. DOI: 10.1161/JAHA.119.015573