This month’s ECG was recorded from a 42-year old male who was complaining of gradually increasing exertional dyspnoea over several months. He was also experiencing breathlessness when lying flat. He had not had any chest pain. Physical examination revealed swollen ankles and feet and a raised jugular venous pressure. Blood pressure was135/90mmHg. There was an apical pansystolic murmur.
Does the ECG provide any clues as to the probable clinical diagnosis?
The Answer
Let’s begin with a systematic description of the ECG, then go on to discuss what it might all mean.
- There is sinus rhythm with a heart rate of about 92 bpm.
- The QRS axis is about 0 degrees, which is within normal limits.
- All the QRS complexes in the limb leads are of low amplitude: none has a total amplitude of more than 0.5mV.
- In the chest leads the QRS amplitudes do not meet the Sokolow-Lyon criterion for LVH, ie S(V1) + R(V5/V6) greater or equal to 3.5mV, but the S waves in V2 and V3 are quite deep. There is also a poor R wave progression in the chest leads with a late transition (V5) to positivity.
- There is widespread, non-specific T wave flattening in the limb leads, and ST depression with low amplitude T waves in V5 and V6.The broad, slightly notched P waves in lead II and biphasic P wave with dominant terminal negative deflection suggest left atrial abnormality.
Let’s consider some of the possible causes of some of these abnormalities:
Highish resting heart rate: heart failure, fever, anaemia, pulmonary embolism, anxiety.
Left atrial abnormality: hypertension, LV systolic dysfunction, mitral valve disease
Widespread ST/T wave abnormalities: myocardial ischaemia, old MI, hypothyroidism, cardiac amyloidosis and dilated cardiomyopathy.
Poor R wave progression: old anterior MI, cardiac amyloidosis and dilated cardiomyopathy.
Now, let’s bring the clinical details of the case into the discussion. The history is not suggestive of coronary artery disease, so old MI or ongoing myocardial ischaemia in this case are unlikely. The blood pressure is normal, ruling out hypertensive heart disease. Although the pansystolic murmur is most likely due to mitral regurgitation, this is not necessarily caused by primary mitral valve disease: it may be secondary to left ventricular systolic dysfunction. Cardiac amyloidosis is a possible cause of several of the abnormalities listed, as well as the clinical features, but such deep S waves in V2 and V3 are not typical of the condition.
As Max pointed out, the combination of low-amplitude QRS complexes in the limb leads (all complexes not more than 0.8mV); dominant S wave in V4; and S(V1/V2) + R(V5/V6) at least 3.5mV is known as Goldberger’s triad, and this is reported to be highly suggestive of a dilated cardiomyopathy.
First described in 1982, Goldberger’s triad is generally reported to have high specificity but low sensitivity(1). This means that most patients with these features will have a dilated cardiomyopathy but the absence of the triad certainly does not exclude the diagnosis.
As we have seen, all the abnormal features of this ECG individually have several possible explanations. However, the total combination of features, whilst not absolutely diagnostic of any condition, is, especially when considered in the presenting clinical context, highly suggestive of a dilated cardiomyopathy. Well done to all those who worked this out. In this case dilated cardiomyopathy was suspected and subsequently confirmed by echocardiography.
- Goldberger A L. A specific ECG triad associated with congestive heart failure. Pacing Clin Electrophysiol 1982;5:593-9.
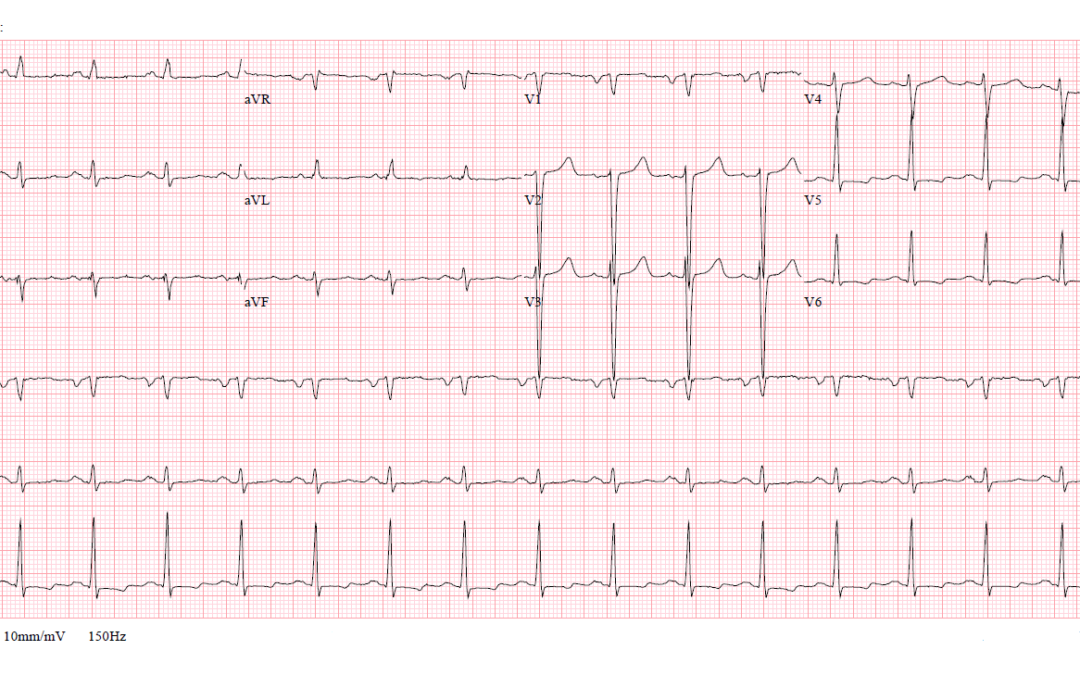
Sinus rhythm. Normal PR interval. Narrow QRS. Appears as normal cardiac axis. Precordial voltage using Sokolow-Lyon criteria (if using V2 and V5) is indicative of LVH. P wave morphology, especially in lead II looks bifid, indicative of Left atrial structural changes; such as dilatation. My knowledge of cardiac sounds is limited but if you’ve got systolic murmur across the entire systolic cycle, does that mean you have MR? It’s likely it’s more MR with this patient. The breathlessness is probably due to blood flow back up into the lungs, causing raised right heart pressures and elevated JVP. Pulmonary HTN/increased RH pressures secondary to MR?
Thanks, James, for some good observations and comments. Strictly speaking there is not LVH by the Sokolow-Lyon criterion unless, as you suggest, you use V2 instead of V1, but your observation is still important. You rightly deduce that there is probably mitral regurgitation, but this raises questions about the possible cause. For instance, is the MR due to primary mitral valve disease or is it secondary to something else? If, the latter, then what could the cause be? Is there anything on the ECG that could help us to answer these questions? And what about the R-wave progression? Is this normal? Are there any other abnormal ECG features not yet mentioned?
The limb lead voltages are quite small whilst some of the precordial amplitudes are quite high which I think is suggestive of DCM. This would also explain a pansystolic murmur due to MR is the mitral annulus is dilated. I think the axis is also on the borderline between normal and left axis deviation
Great comments, Katie! To everyone out there – is there anything more to be added to the description and interpretation of this ECG?
Sv4+SD>2.8mv, Rv6/Rmax>3,> LVH? ptfv1<-0.04, DCM?
Thanks for your comments, Kun, which certainly have the merit of brevity. Unfortunately I don’t know what all your abbreviations mean but I do understand your concluding tentative diagnosis. I’ll wait a few more days before I add my own comments.
I’d agree with DCM based on presentation.
ECG wise borderline LAD, Bifid in II, and poor R-Wave progression from V4-V6, and the ST abnormalities in the lateral leads stand out. Could the last 2 criteria suggest an old anterior MI or possible early acute ischemia?
Thanks, Dillon. You’re right to draw attention to the poor R wave progression. Although this is commonly due to old anterior MI, there are several other possible causes. The history and ECG together don’t really point to acute ischaemia, so I think, by considering all there various factors together, we are arriving at a probable diagnosis.
As others have mentioned the findings are increased voltages in the chest leads with small voltages in the limb leads. Appears to be evidence of left atrial abnormality – difficult to see the P wave in lead II but there is a large negative P wave in V1. There are also some ST/T changes and poor R wave progression (the QRS complex is not positive until V5). As everyone says, I think this is all suggestive of dilated cardiomyopathy of which there are various causes and would also explain the murmur. There is a set of findings known as Goldberger’s triad:
1. The QRS amplitude in each of the limb leads doesn’t exceed 8mm.
2. The S wave in V1 or V2 plus the R wave in V5 or V6 is equal to or exceeds 35mm.
3. In V4 the S wave is bigger than the R wave i.e. an R/S ratio of <1.
Not every patient with DCM/heart failure will have these changes and I can't remember the sensitivity/specificity. I think the theory is that a large poorly functioning LV causes ventricular electrical activation to shift more posteriorly. You still get LVH in the chest leads (on the horizontal plane) but the transition to positive QRS doesn’t occur until V5/V6. The posterior shift is not picked up very well by the limb leads because they lie in the vertical plane, hence the small voltages. Not sure if that theory is correct though, so over to Dave!
Thanks, Max. I don’t think you’ve left me much to say!