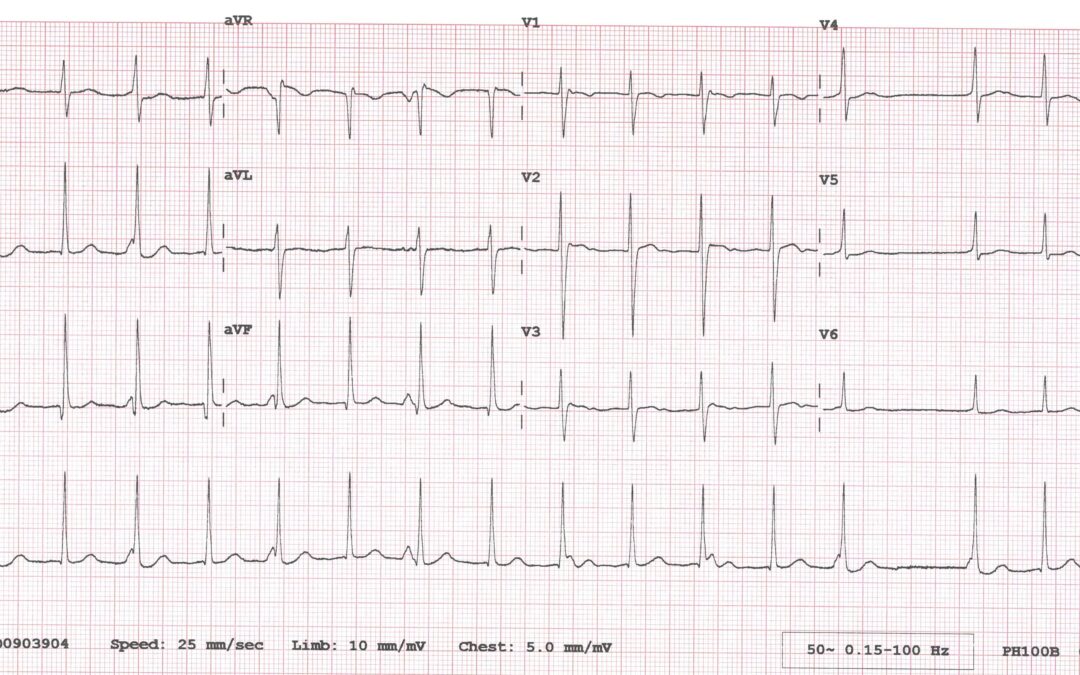
The only information I have about this case is that the ECG was recorded from a 10-year-old child, but my question is a simple one: what is the rhythm? Please describe exactly what you think is happening.
The Answer
Well, this one elicited quite a few responses, with several different explanations proposed.
I have tried to illustrate what I think is happening in the below laddergram that accompanies the rhythm strip (RR intervals shown in milliseconds).
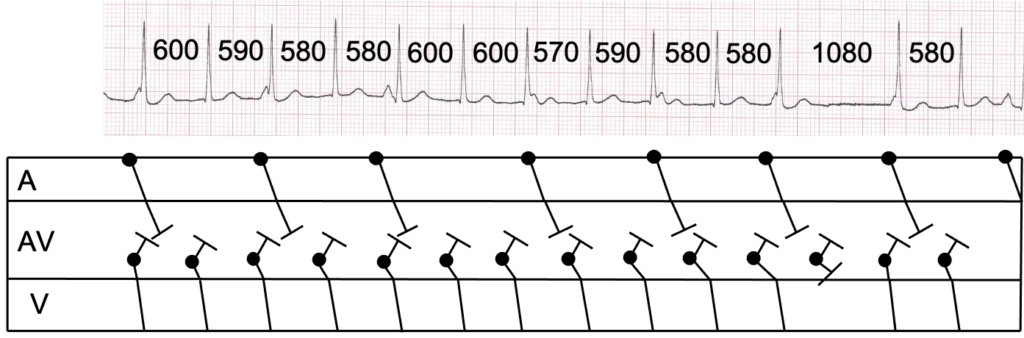
It’s often useful when trying to solve an arrhythmic puzzle to start with identifying all the atrial activity. Here we have P waves that are positive in leads I and II and that occur at a rate of about 50/minute but are slightly irregular. There is therefore an underlying sinus bradycardia/arrhythmia. Some of these P waves fall immediately before QRS complexes, perhaps creating the impression of delta waves; some occur immediately after, resembling J waves. But they are all P waves, and this brings us to one of key abnormalities of the rhythm: there is AV dissociation.
The ventricular rate is, for the most part, just above 100 bpm and the QRS is narrow. I think this is because there is a junctional ectopic, or non-reentrant junctional, tachycardia. I don’t think this is an AVNRT because of the relatively slow ventricular rate and the presence of AV dissociation: in AVNRT there is a common upper pathway that makes retrograde block, and therefore AV dissociation, very unlikely (1).
Although the tachycardia is almost perfectly regular, there is a pause in the ventricular rhythm that is just under two normal RR intervals in duration. A possible explanation for this is that there is Wenckebach exit block from the junctional focus. This phenomenon has been reported previously, although it seems that it is usually caused by digitalis toxicity (2).
An interesting side-issue is the sinus bradycardia in a 10-year-old child. As Scott ingeniously suggests, this may be an automatic reaction to the junctional tachycardia, a circulatory system reflex that aims to correct the abnormally high cardiac output. We often see the opposite of this in complete AV block, where there is a reflex sinus tachycardia in the presence of a slow escape rhythm.
None of the P waves in this ECG conduct to the ventricles, so is there any heart block? No, none at all. The reason that none of the sinus impulses conduct is simply because they always arrive at the AV node when it is in its refractory state due to the rapid junctional discharges. The failure to conduct in these circumstances is physiological rather than pathological.
Please feel free to continue to comment on the ECG and my explanation.
I am grateful to everyone who has contributed to the discussion and to Su Baxter for sending me the ECG.
- Alasti M, Mirzaee S, Machado C et al. Junctional ectopic tachycardia (JET). J Arrhythm 2020;36(5):837-44. DOI: https://doi.org/10.1002/joa3.12410.
- Barold SS, Hayes DL. Non-paroxysmal junctional tachycardia with type I exit block. Heart 2002;88(3):288. DOI: http://dx.doi.org/10.1136/heart.88.3.288.
Sinus bradycardia with junctional tachycardia? if that’s even possible
Thanks, Jamie. Just because something is unusual doesn’t mean it’s not possible! I won’t comment at this stage but would just ask if you can think of any reason why the tachycardia stops then starts again in the way that it does.
P-P interval is consistent throughout, the R-R interval during the pause is roughly twice what it is before and after, suggestive of a sino-atrial block which would help explain the sinus bradycardia too. At 10 years old I think a resting heart rate of around 100 would be fairly normal due to the higher excitability of the cardiac cells at that age, I often assume ECG’s this strange would be due to drug overdose/side effects, but being paediatric, the ECG’s are often strange to me
Thanks again, Jamie. Are you saying that the apparent sinus bradycardia is actually sinus tachycardia with 2:1 SA block? And how would this be related to the pause if, as you say, there is also a junctional tachycardia?
This is WPW tachycardia, with T wave abnormality.
Thanks, Frederick. Why do you think there is WPW?
I have a feeling that considering the age, absent p waves, j waves abnormality and delta wave.
Thanks for expanding on your original comment, Frederick. I think my questions would be: are there really no P waves, and are there really J some waves and delta waves? The questions are linked!
I think this is an atypical presentation of AVNRT, which lacks retrograde conduction so allows the concurrent sinus bradycardia to walk through, and at least once blocks anterogradely in the His bundle, causing the ‘missing’ R-wave and doubled RR interval.
Thanks, Scott. An interesting suggestion. I’m going to have to think about this one, and maybe do a bit of reading too.
I’m assuming that the patient is already beta-blocked, which would go some way to explaining the relatively slow atrial rate, slow ventricular rate, and retrograde block.
I don’t know if this child was beta-blocked, but would a beta blocker cause an AVNRT to have a relatively slow ventricular rate?
Beta blockers can lengthen PR interval in normal conduction, by their effect on the AV node – my assumption being the effective creation of a slow-slow circuit.
This could of course also more simply be an ectopic/automaticity/focal tachycardia located in the upper His bundle (allowing for anterograde block to occur), for which the ventricular rate is more typical. Compensatory parasympathetic tone resulting from the homeostasic mechanism may also explain the slow independent atrial rate.
As usual I wish I thought of this before reading Scott’s answer
Sinus bradycardia of 56bpm with subtle sinus arrhythmia
Ventricular rate of just over 100 (ignoring the dropped beat)
There appears to be complete AV dissociation, I would have thought too fast for an AV node escape rhythm, but I don’t know if being 10 might change that?
I think Scott’s answer of AVNRT without retrograde atrial conduction would make sense, and a cursory glance at literature summaries show slower AVNR arrhythmias, so that could also fit.
I don’t really understand why the conduction would be so impaired to give complete retrograde block, with occasional anterograde block, a fairly slow AVNRT and sinus bradycardia in a 10 year old.
Thanks for your comments, Jon. I also am not sure why there might be retrograde block from an AVNRT, so I’ll see what I can find out on the subject.
Thanks for your further comments, Scott. It’s always interesting to read and ponder on your explanations.
Atrial tachycardia with Delta-wave presence
Thanks for your comment, Verona – we’re getting good variety of opinions now. Are you sure what you’re seeing is a delta wave? Is it consistently present?
Wrong about delta wave 🙂
Wandering atrial pacemaker..?
Thanks, Jennifer. Yet another suggestion! This is obviously not a simple, straightforward ECG.
Junctional bigeminy pattern with two foci in ?
Thanks Kale. I have to admit that I can’t see a bigeminal pattern. The tachycardia appears regular to me (apart from the pause), although I haven’t yet made precise measurements.
Looks like a Junctional Escape-capture bigeminy or escape-echo bigeminy..
Thanks for your comments, Verona. Escape beats occur after a pause so I’m not sure which you think are escape beats here. Also, I confess that I can’t see a bigeminal rhythm, but perhaps I’m not looking closely enough!
On lead ||clear pattern of two different morphology junctional beats:
Beats 1,3,5,7,9,11,13 are merged with retrograde p-wave
Beats 2,4,6,8,10,12 without p-wave
Best 14 is missing and interval R-R beats 13-15 twice longer preceded R-R
Accelerated junctional rhythm with sinus pause
Thanks for your comment, Olalekan. You say there is a sinus pause, but does the sinus node actually pause or does it continue without interruption?
…but are the P waves definitely retrograde?
No retrogrde Pwave .
The comments have got a bit out of sync. My question was in response to Verona’s last post.
It looks like isorhythmic AV dissociation? It looks the sinus rate has slowed down and the junctional rate is accelerated?
Thanks, Michelle. I agree that that it looks like there is AV dissociation, but perhaps it’s not ‘isorhythmic’. This term is normally used to describe the situation where junctional and sinus node discharge rater are almost identical so that the AV node and sinus node are ‘competing’ for control of the ventricles, with the AV node usually ‘winning’ because of a slightly higher automatic rate.
Interesting case with a great explanation and laddergram as ever. I’ve only seen cases of juctional exit block in textbooks/papers. Perhaps partly because Digoxin seems to be used less frequently?
Yes, Arron, I’m sure that’s a factor, but I’m sure it was pretty rare anyway and it probably goes unrecognised most of the time anyway.