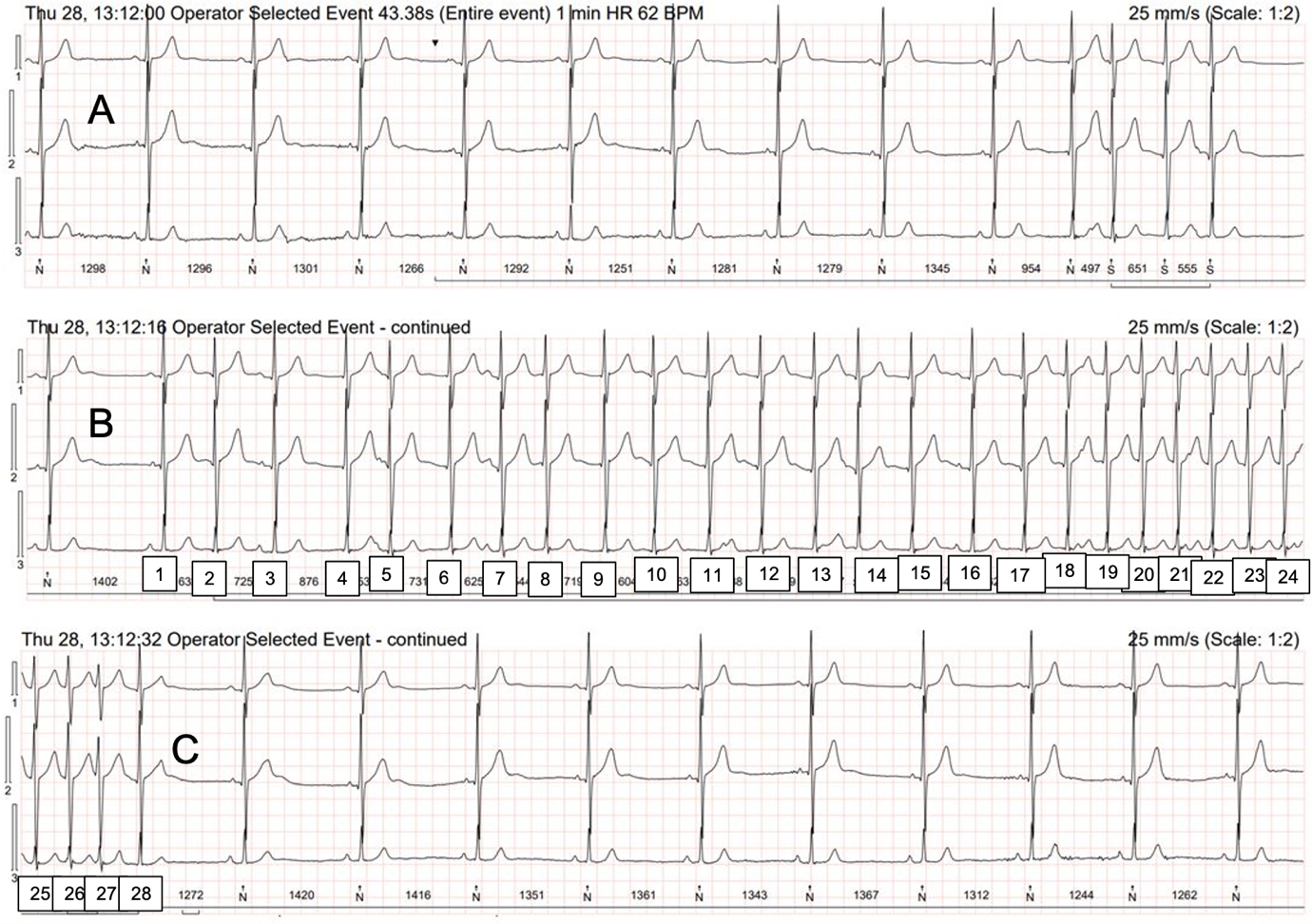
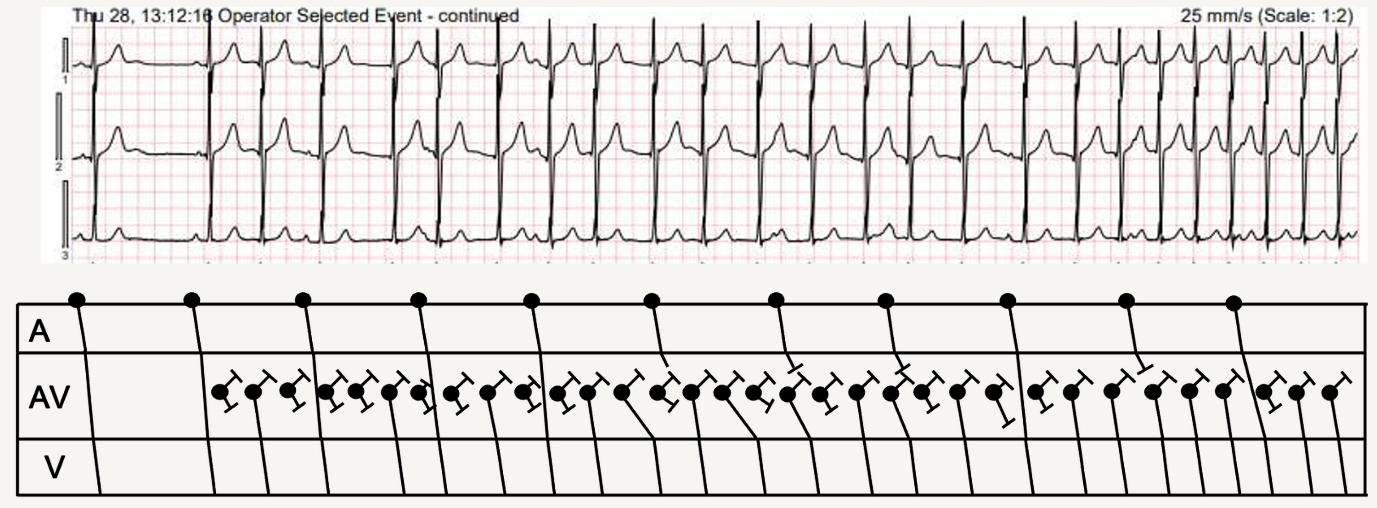
This month’s ECG comes courtesy of Scott Walton, arrhythmia afficionado and regular contributor to our discussions on this page. This is a 32-second extract from a Holter recording from an elderly male who had suffered a stroke and was being screened for paroxysmal atrial fibrillation. I am happy to admit that I don’t know exactly what is happening here. Concentrating on the middle section, I can see that the rhythm is mostly irregular, although fast and regular towards the end, and that there are some obvious P waves, but I can’t work out the relationship, if any, between P waves and QRS complexes and why the rate is mostly irregular.
What do you think is happening?
_____________________________________________
‘AN’ ANSWER
NOTE: Answer added 19.02.24
The provider of this month’s ECG, Scott Walton, has supplied us with a detailed explanation of what he thinks is happening. Do you agree with it? Do you have an alternative explanation or anything further to add? I haven’t made up my mind yet but will add a few comments of my own in a few days’ time.
Dave Richley
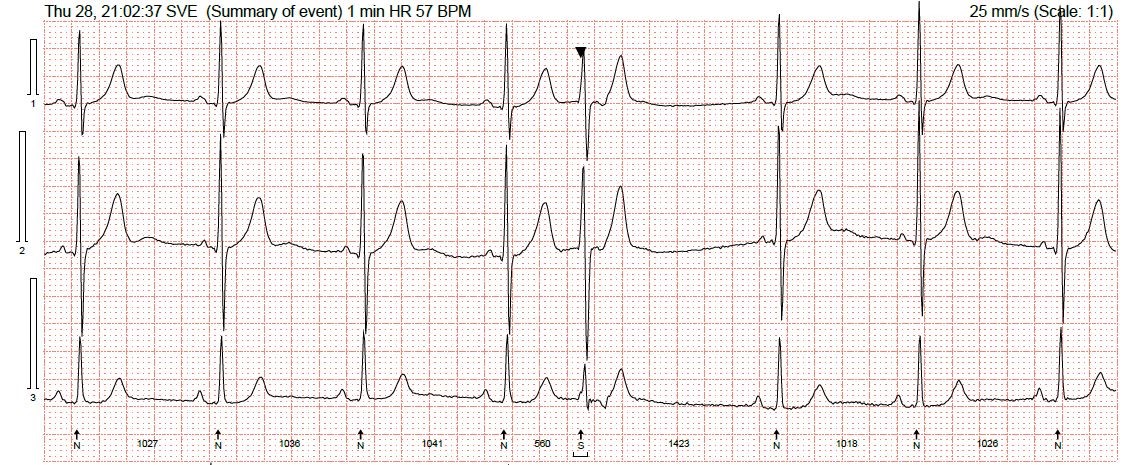
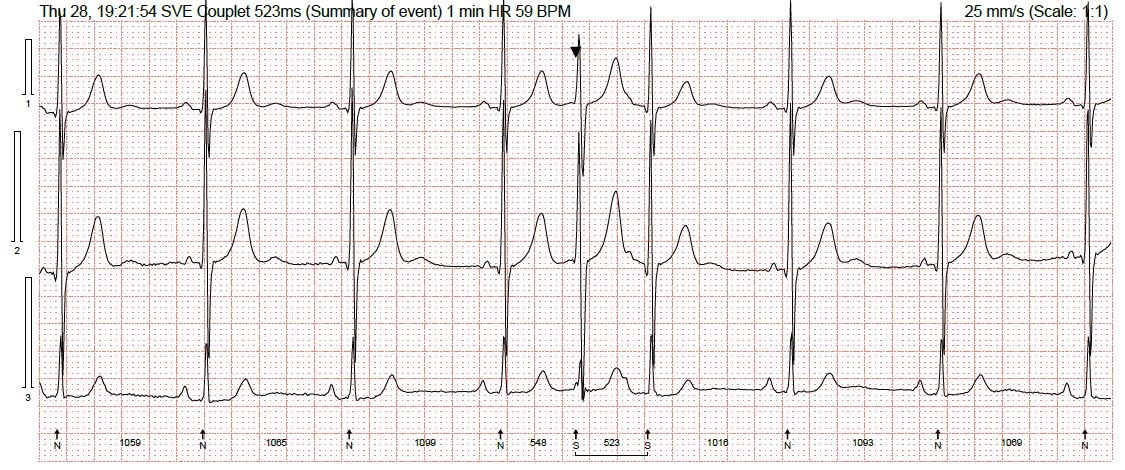
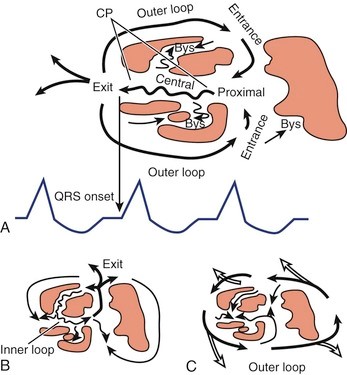
Apart from the QRS morphology, everything about this is consistent with a short ventricular arrhythmia, particularly having independent and entirely uninterrupted atrial rhythm. If this had been detected by a pacemaker or ICD it would be discriminated as ventricular simply as there are more V’s than A’s. The irregular onset followed by acceleration and stabilisation is a pretty typical pattern for NSVT with a fibrotic/scar substrate, and in pacing clinics we see this regularly. Just like:
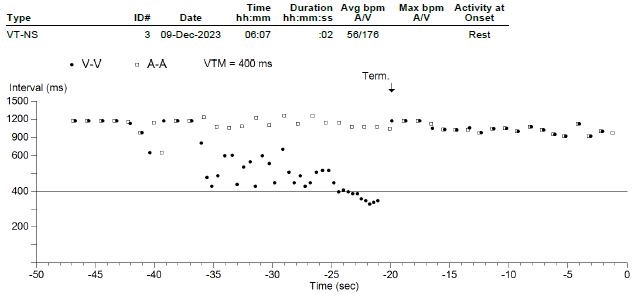
The complete lack of retrograde conduction would be unusual for a supraventricular arrhythmia. AV conduction of sinus P-waves is also barely affected, implying the AV node is not involved with propagating or sustaining the arrhythmia.
We don’t often think about narrow complex ventricular arrhythmias, as they contradict one of the first things we learn: VT has a broad QRS. Some studies indicate that almost 5% of VT is actually narrow QRS (https://www.acpjournals.org/doi/abs/10.7326/0003-4819-114-6-460). My feeling is that the prevalence in practice isn’t really this high, but I could be wrong, or perhaps just assumed they were all SVTs with some degree of intraventricular aberration.
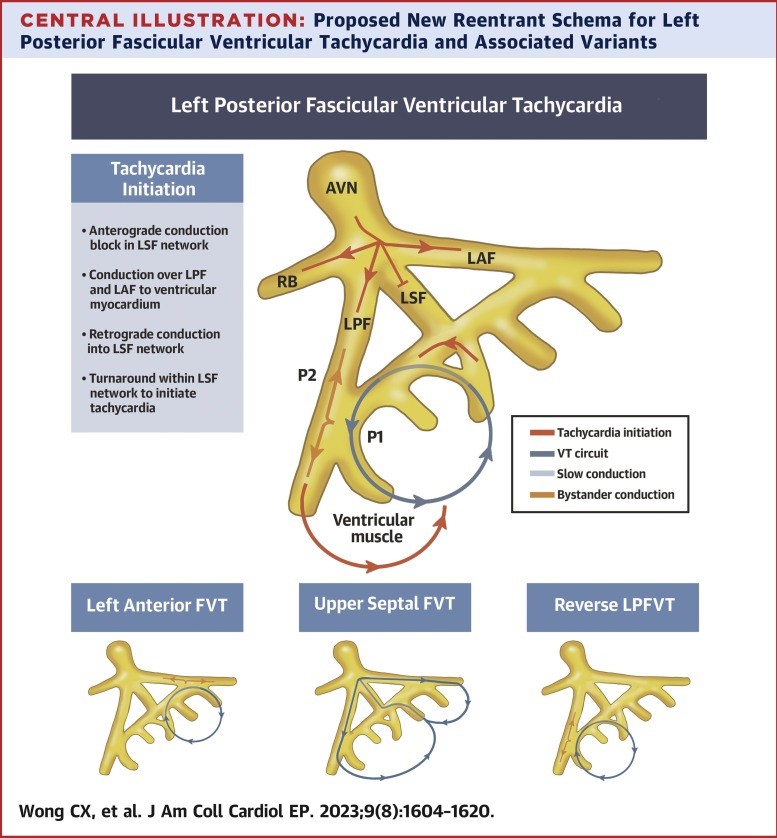
There are plenty of mechanisms that could explain the pattern seen here, as almost any imaginable variant of accessory pathways exist, alongside a micro-re-entrant scars and fascicular re-entry. The most comparable case study I found was this:
Although the QRS of conducted sinus complexes is narrow, it isn’t necessarily normal (relatively deep S-wave, although of course I have no idea where the ECG electrodes have been placed), and therefore could represent a hemi-block, which could represent either a substrate for arrhythmia, or a conduit for ventricular rhythms to enter the intraventricular conduction system by the same pathway as anterograde supraventricular activity, by travelling retrogradely up the “blocked” fascicle, then anterogradely down the normally conducting fascicles.
There are also slight morphological QRS differences between those beats which are normally conducted and the ectopic complexes, although they are not particularly telling, or even consistent. I’ve included a couple of the other narrow complex isolated premature beats found on this recording, both of which display characteristics consistent with ventricular ectopy, although they do have a slightly slurred/notched initial deflection which is only partly seen in the actual arrhythmia towards the end as the rate accelerates. One of these isolated ectopic beats also displays complete retrograde conduction, whereas the interpolated complex has incomplete retrograde conduction, which is the same as the arrhythmia.
To summarise my theory, I think there is an area of scar with at least two possible micro-re-entrant circuits, which is either alongside the His bundle, or is able to conduct retrogradely up one anterogradely blocked fascicle to then conduct through the other bundle branches in virtually the same way sinus complexes do. The only way to confirm the pathways involved would be a full electrophysiology study, however this arrhythmia is not sustained or symptomatic, so invasive investigations are not indicated or justified to clarify the mechanism involved.
Scott Walton
_____________________________________________
COMMENTS FROM DR RICHLEY
NOTE: Added to site 22.02.24
I find this one difficult, but there are a few things that I think I can be confident of, so let’s start with those and then try to work out what might be happening with the rest of the ECG. There is an underlying sinus bradycardia and this continues through the periods of ventricular irregularity as well as the regular tachycardia. This means that whatever the source of the non-sinus beats, there must be retrograde block so that the sinus node can continue to function without interruption. It is very possible, even likely, that during the arrhythmias at least some of the sinus P waves are conducted, but it’s difficult to be sure exactly which are conducted and which just happen to occur before a QRS of ectopic origin.
So, what is the origin of the non-sinus beats and what might be the mechanism(s) behind their appearance? The non-sinus QRS complexes are narrow and of almost identical shape to the sinus complexes, so are almost certainly of AV junctional origin. However, the AV junction is generally understood to comprise the AV node and the bundle of His, perhaps including also tissue immediately adjacent to the AV node, so identifying the origin as junctional doesn’t really pinpoint it precisely. Towards the end of strip A and for the first 17 beats of strip B there are complexes that are not preceded by P waves. The coupling intervals vary, making the heart rate irregular. Are these irregularities due to sinus rhythm with multiple, random premature discharges from an ectopic junctional site, or could they be due to an irregular, automatic junctional tachycardia that shows a ‘warming-up’ phenomenon before it evolves into the faster and more regular tachycardia that is seen from beat 18 to beat 28?
Maybe, as Scott suggests, this is a rare narrow-QRS re-entrant ventricular arrhythmia due to myocardial scarring – I just don’t know. Alternatively, could there be an automatic junctional tachycardia with retrograde block and variable exit block, such that not all the junctional impulses emerge from the focus, perhaps associated also with variable AV block, to explain the irregularities of rate? Again, I don’t know but I have created a laddergram to show how this might provide an explanation for what we see. This is highly speculative, and quite likely to be completely wrong, but it shows a junctional site discharging at a rate of about 150 bpm, but with initially many impulses failing to propagate to the ventricles because they fail to conduct out of the junctional focus (exit block) or through the AV node (AV block). There is also entrance block, meaning that the junctional focus is immune from depolarisation from the sinus impulses, so that it continues to depolarise at a regular(ish) rate. This, as suggested by Arron Pearce, would be a parasystolic mechanism. In this explanation, some of the sinus impulses manage to conduct through to the ventricles and some of them don’t, which explains some of the ventricular irregularity.
There are probably other plausible – and better – explanations. I have previously quoted the legendary arrhythmia expert, the late Dr Mauricio Rosenbaum, and I make no apology for doing so again: “Every complex arrhythmia has at least 3 different explanations!”.
I wish to thank everyone who has participated in the discussion, but particularly Scott Walton, who not only supplied the ECG but also provided a detailed, referenced explanation. Further contributions are welcome.
Dr
Sinus Rhythm–Paroxysmal AFIB– Sinus Rhythm
Thanks, AIDHA. Are you sure about the AF? I think I can see dissociated sinus P waves.
Atrial run
In the context of a recent stroke, treat as paroxysmal AF. Don’t go down rabbit hole of treating the ECG and not the patient.
Quite right, Mags, although for this particular exercise we are primarily concerned with trying to understand the ECG.
Maybe multifocal atrial ectopy +|_ atypical flutter?
Thanks, Mags. Multifocal atrial ectopy would require premature P waves of different shapes and I’m not sure we see that here. In fact, it could be argued that there are no premature P waves at all! Again, I don’t think the evidence of atrial activity supports a diagnosis atrial flutter. At this point I think I’m more confident in saying what I think it isn’t rather than what it is. This is not straightforward!
Very interesting ECG.
Looks like possible interpolated junctional ectopics with couplets, triplets and then a tachycardia further down the trace. Probably minimal retrograde activity and a fairly slick conduction system.
Yes, it is interesting, Ahmed, and I think you’re on the right lines.
Poured over this one for a while…
I think sinus P waves (sinus arrhythmia) march through the tachycardic segment and there is a ? junctional (parasystolic) rhythm that eventually speeds up into a JT.
There’s probably another explanation, maybe even a simpler one.
Thanks for adding to the discussion. Can a junctional parasystole speed up into a junctional tachycardia, approaching 150/min, and then suddenly stop? I just don’t know. Could there initially be variable exit block rather than a slower discharge rate? It’s certainly an interesting and challenging ECG.
Thanks for adding to the discussion. Is it likely that a junctional parasystole could start off slowly, accelerate to a rate of nearly 150/min, then just stop suddenly? I just don’t know. I’m wondering if there could be variable exit block from a junctional focus and that the increase in rate is due to a reduction in this block rather than an increase in the discharge rate. Again, I don’t know but I’m working on a laddergram to see if this might be at least theoretically plausible.
*Pored over
Junctional premature contractions
Thanks. What do you think the tachycardia is? Also, which beats are JPCs and which are sinus beats?
Without being able to measure, the p waves are going at their own rate similar to the atrial rate whilst in sinus rhythm.
?dissociation between the rate of SA electrical signals and AV signals.
? An Accelerated junctional escape rhythm or junctional tachycardia with dissociation
Thanks, Chrissie. Yes, I think there is a junctional tachycardia with AV dissociation but I’m not sure I can yet provide a complete explanation for the irregular section.
I see sinus bradycardia with a parasystolic, automatic junctional rhythm which causes intermittent AV dissociation. The junctional rhythm starts of slowly (“warming up”) but increases in rate to a junctional tachycardia. You can map out the fairly regular sinus P waves throughout tracings A, B and C – the junctional rhythm initially falls in between sinus conducted beats without effecting the sinus rate.
Looking more closely at strip B and C – most of the P waves are still able to conduct to the ventricles: beats 1,3,5,7,14 (P hidden in T),16,28 are sinus conducted beats whereas beats 9 (P hidden in QRS),11,18,21,24 contain P waves that are not able to conduct to the ventricles as the AV node is still refractory. Most sinus conducted beats have no S wave in channel 3 whereas the junctional beats do have small S waves. Perhaps the sinus beats with small S waves (beats 5 and 7) represent a degree of fusion between the junctional rhythm and sinus conduction.
At the start of C we can see a hidden P wave in channel 2 just prior to QRS 28, this is a sinus conducted beat which restores sinus capture with termination of the junctional rhythm. Sinus bradycardia then continues with normal AV conduction.
Thanks for an excellent assessment of what’s visible on the ECG.
From where within the “junction” might this arrhythmia arise given its minimal effect on AV conduction of sinus beats, and are we thinking ectopic arrhythmia, or perhaps something micro-re-entrant?
Thanks for this detailed explanation, Arron. I probably agree with most, if not all, of it but I’m not yet certain I have a full understanding of the arrhythmia. One thing I’m struggling to understand is which beats are sinus-conducted. I agree with you that beats 1, 3, 5 and 7 certainly look like sinus beats, but what about beat 12? Could this be conducted with a long PR interval? The same question applies to some other beats. If beats 4 and 8 are both of junctional origin, why does beat 4 emerge after a relatively long RR interval of 920 ms, whereas beat 8 appears early after only 560 ms? Could some of this irregularity be explained by varying exit block from a junctional focus? If so, maybe it’s a reduction in the amount of exit block rather than an increase in the rate of automatic discharge that explains the apparent increase in the rate of the junctional tachycardia. I’m currently working on a laddergram to see if this seems plausible. You mention that the junctional beats tend to have a small S wave in channel 3, whereas the sinus beats do not, but I wonder if the presence or absence of an S wave is simply a function of the rate rather than the site of impulse origin – complexes with an S wave tend to end a short RR interval and may therefore represent slight rate-related aberrancy.
I think we’re getting there but maybe there’s still a little bit of work to do. I’ll keep thinking!
Beats 14 and 28 argue against rate related aberrancy, as both appear to be sinus conducted complexes with a shorter RR than the preceding interval, yet lack said S-wave in channel 3.
I think it could be argued that beat 28 follows an RR interval that is relatively long compared to the preceding few RR intervals, but what you say about beat 14 is certainly true and does undermine my theory.