I wish to thank Arron Pearce, cardiac nurse and ECG analyst, for this month’s case. It concerns a 30-year-old male who presented with dizziness, chest tightness and palpitations. Figure 1 shows the presenting ECG and figure 2 a follow-up ECG recorded a few weeks later.
Please note: all of the limb leads in the 12-lead display show the same 2.5 seconds of ECG. The rhythm strip shows a sequential 10-second recording of lead II.
What is your diagnosis? Please provide your reasons.
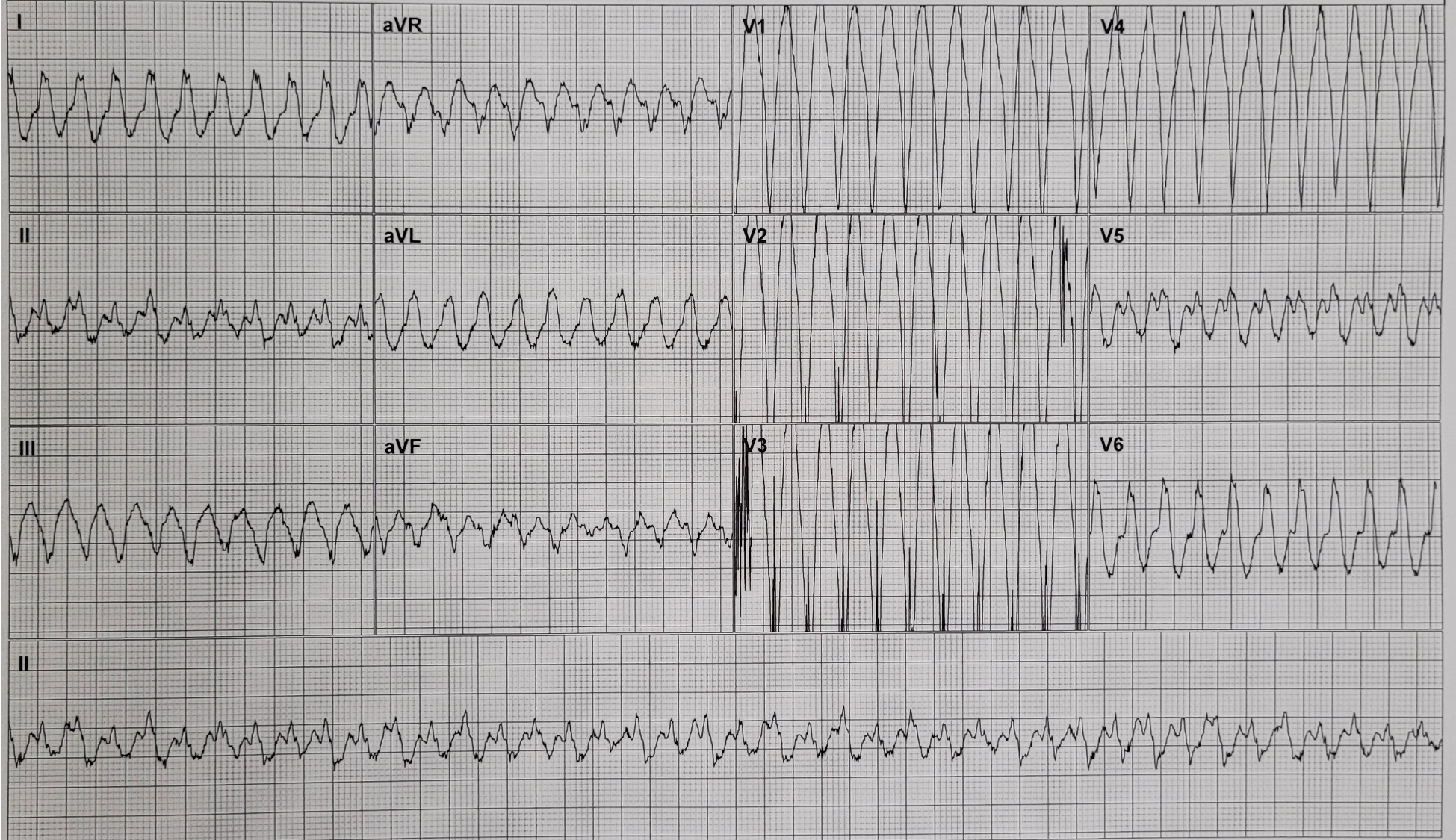
Figure 1: Initial ECG recorded during chest tightness, dizziness and palpitations
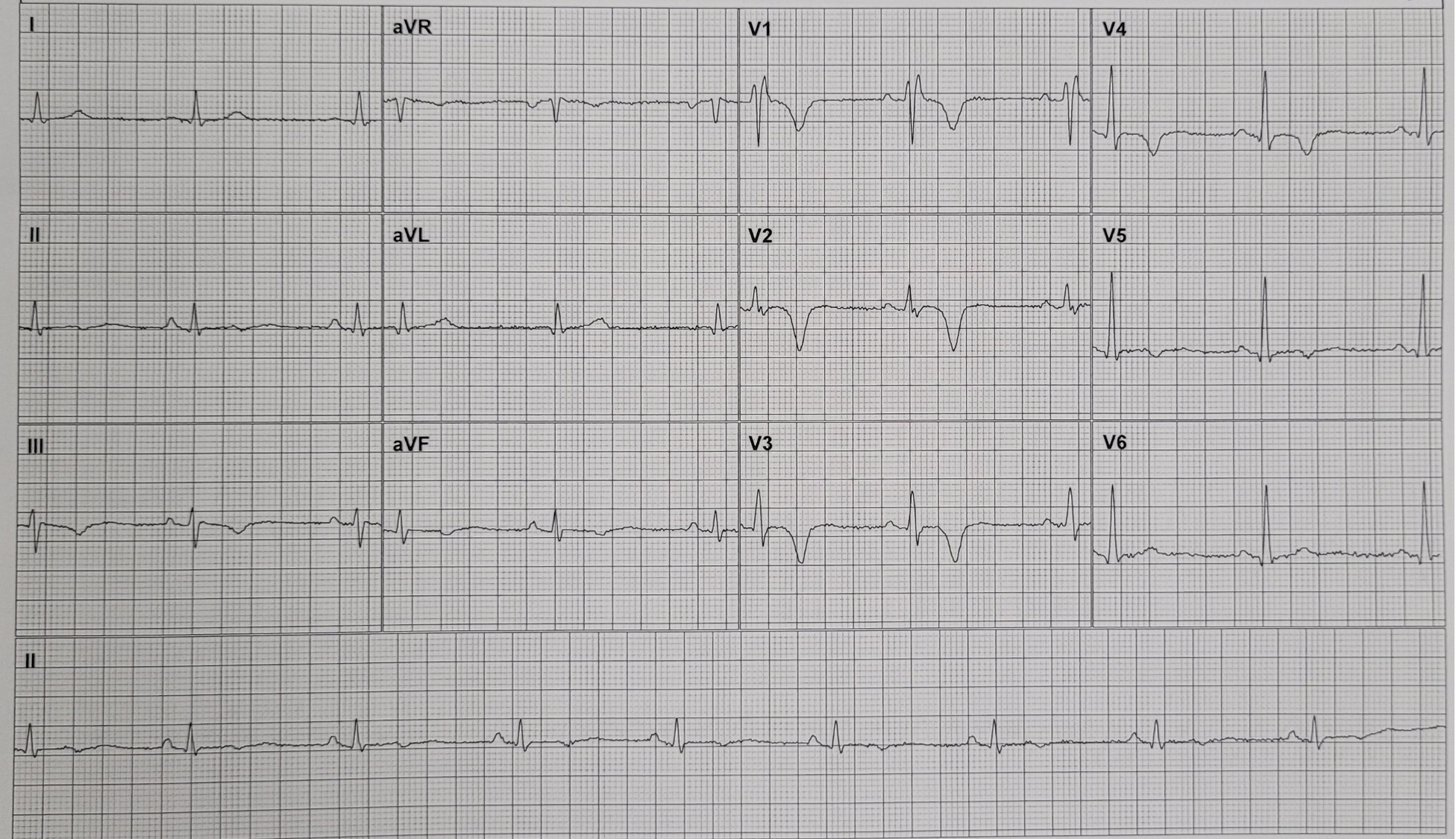
Figure 2: Follow-up ECG recorded a few weeks later
ANSWER
NOTE: Answer added 21.03.24
We’ll start with the first ECG. This shows a regular, broad-QRS tachycardia at a rate of 250 bpm and the assumption must be that this is VT. But there is more we can say about the ECG. The QRS has a LBBB morphology, which means that the tachycardia originates from the right ventricle. One tachycardia that has a LBBB morphology is right ventricular outflow tract (RVOT) VT. This is the most common of the so-called idiopathic VTs – relatively benign tachycardias that occur in people with structurally normal hearts – but RVOT VT is characterised not only by a LBBB morphology but by an inferior QRS axis too, and that’s not what we see here. Here the QRS axis is about -30 degrees, so the ventricular forces are directed somewhat to the left rather than inferiorly. The tachycardia therefore originates in the RV, but not the RVOT.
Let’s now move on to the second ECG. This shows sinus bradycardia at 53 bpm with normal QRS axis, T wave inversion in III and aVF, a biphasic T wave in II, and T wave inversion from V1 to V5. There is also an rSr’ complex in V1, with a duration of 120 ms; a very small positive deflection after the R wave in V2; and a slightly slurred upstroke to the S wave in V3 and V4. What is the cause of the wide rSr’ complex in V1? It would be easy to attribute this to RBBB, but the T wave inversion here is far more extensive than we would expect to see in RBBB. In RBBB there is normally T wave inversion in those chest leads where the 2nd R wave is dominant – usually only V1. So, if this is not RBBB, what is it? This is a case of arrhythmogenic right ventricular cardiomyopathy (ARVC), a progressive, genetic condition in which healthy RV myocardium is replaced by fat or fibrofatty tissue, with myocardial inflammation and scarring and loss of contractile function. This can result in segmental aneurysmal dilation of the RV, with the areas of RV disease providing foci for potentially lethal ventricular arrhythmias. In many, if not most, cases there is involvement of the left ventricular myocardium as well, and evidence of this is provided by widespread T wave inversion.
The patchy RV disease causes delayed depolarisation of areas of RV myocardium, resulting in late deflections on the end of the QRS in chest leads that overlie the RV. A small positive deflection on the end of the QRS, as seen in V2 in figure 3, in ARVC is known as an epsilon wave but the delayed RV depolarisation can also cause a slurring or ‘jerkiness’ of the upstroke of the S wave, as seen in V3 here. The second R wave in V1 could be regarded as a big epsilon wave since it also is due to delayed RV activation, and the reason the QRS in V1 is similar to that seen in RBBB can easily be understood if we recall the reason for the typical QRS morphology in V1 in RBBB. In RBBB, because of a conduction abnormality, depolarisation of the RV is delayed and prolonged, resulting in a tall, broad second R wave. In ARVC, because of disease of the RV myocardium, depolarisation of regions of the RV is also delayed and prolonged and this may lead to an epsilon wave or a second R wave in V1.
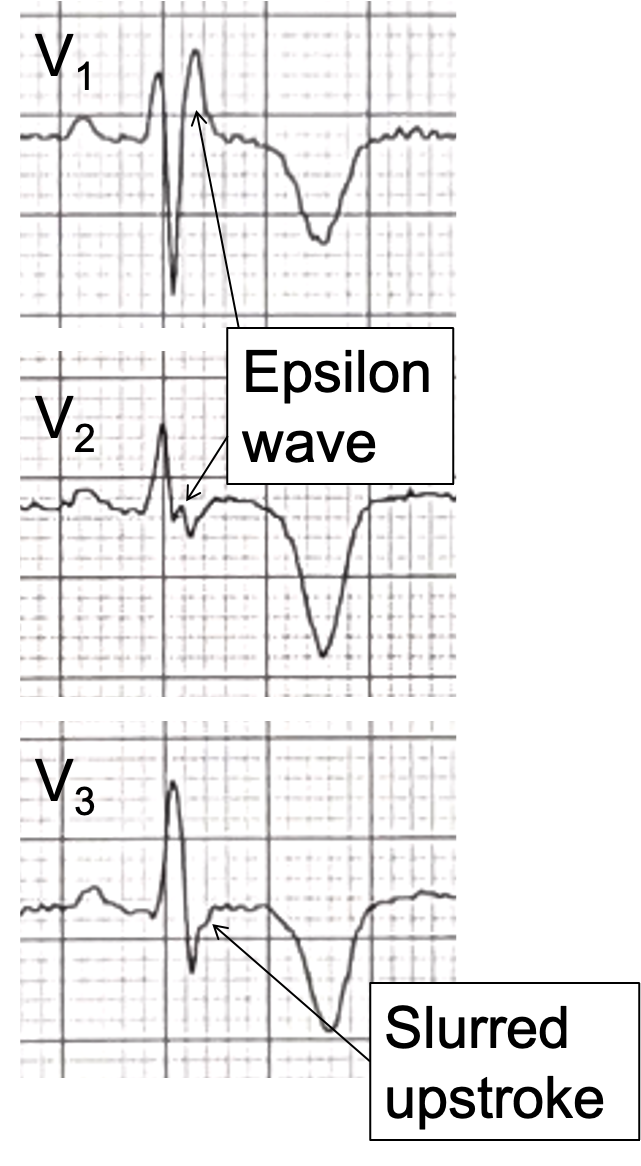
Figure 3. Close-up of V1-V3, showing evidence of delayed RV depolarisation.
The diagnosis of ARVC was confirmed in this patient and he received an implantable defibrillator to prevent arrhythmic sudden death.
Thanks again to Arron Pearce for supplying the ECGs and clinical history, and to everyone who participated in the discussion.
Dave Richley
First ECG – ventricular tachycardia
Second ECG – RBBB
Thanks, Iyesha. Yes, the first ECG shows VT and the 2nd ECG certainly does shave some features of RBBB, but is it really RBBB, or are there reasons for thinking it might be something else?
The 1st ECG shows a regular wide complex tachycardia at approximately 250bpm. I can’t see clear evidence of P waves, but I’m making the assumption that it’s ventricular tachycardia. The 2nd ECG shows sinus bradycardia at around 56bpm, normal axis, with abnormal T wave inversions in the precordial leads V1-V5. The R wave height also seems large in the anterior chest leads, which suggests RV hypertrophy. Taking it all together with the history, I also suspect arrhythmogenic RV cardiomyopathy but am happy to be corrected on anything I have missed or misinterpreted!
Thanks, Leah. Your assumption that the 1st ECG shows VT is a very sound one – it’s always best to assume that a regular broad QRS tachycardia is VT unless there is good evidence to the contrary. Your reasoning about the clinical diagnosis, taking account of both ECGs and the clinical history, also makes perfect sense. I’ll post my full description soon.
Comment is it arrythmogenic cardiomyopathy? Wide qrs RBBB. The epsilon waves in v1-v4
Thanks, Debbie. You might be on to something here. I’ll provide my full analysis in a few days’ time.
The first ECG looks like vent ventricular flutter dur the high heart rate and monomorphic waves
The second one looks like a an arrythmogenic right ventricular dysplasia . We can see epsilon waves in V1-V2 maybe?
Thanks, Vânia. I think I would describe it as ventricular tachycardia rather than flutter, albeit a very fast VT, but I certainly agree with your other observations.
a broad complex tachycardia followed by possible Wellens Type 2
Thanks, Alex. Yes, there is a broad complex tachycardia, but what is its origin and how might it relate to the follow-up ECG? Wellens is certainly one possible cause of T wave inversion but there are many others and to diagnose Wellens you really need to see a dynamic pattern in which the ECG changes with the symptoms.
Taquicardia ventricular en el primer trazado. El segundo trazado con ondas epsilon en precordiales y empastamiento de S, inversión de T en precordiales y DIII configuran diagnóstico de cardiomiopatía arritmogénica.