These ECGs (figures 1 and 2) were recorded during an exercise tolerance test on a man who was being investigated for an episode of collapse and paroxysmal tachycardia. What is the explanation for the transient change in QRS morphology?
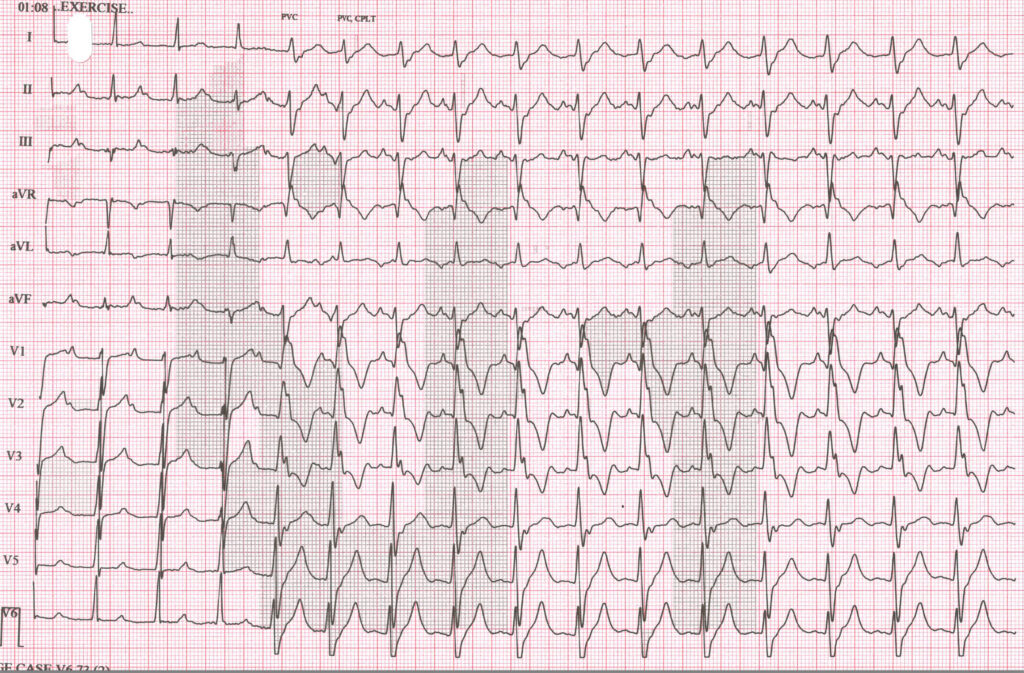
Figure 1
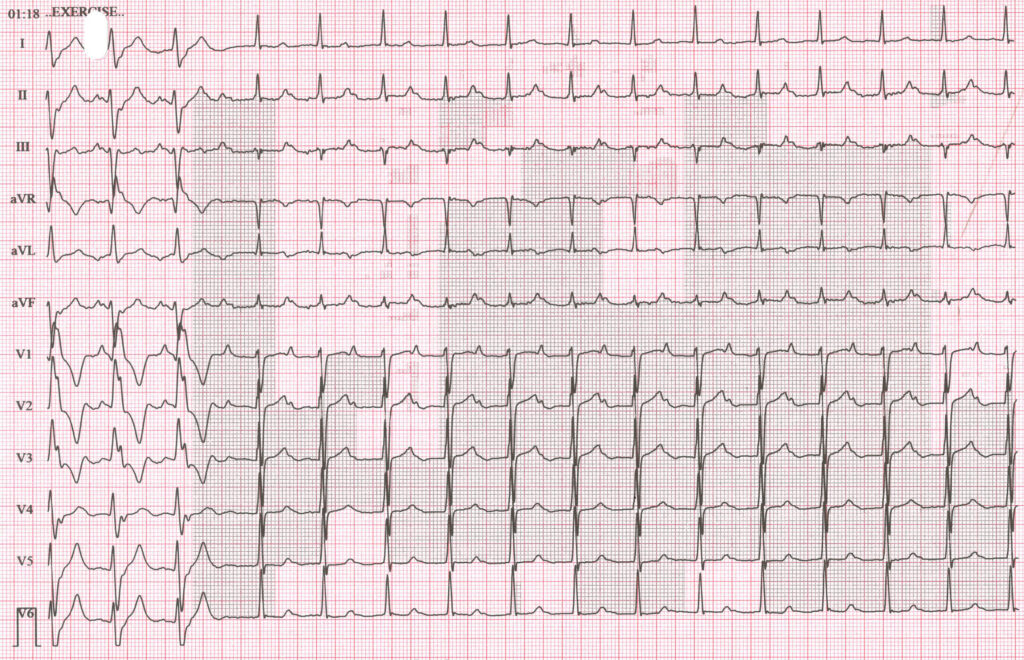
Figure 2
I wish to thank Debbie Wilson and Klara Powell of Mid Yorkshire Teaching Trust for sharing this case with me.
The Answer
The ECG begins with sinus rhythm at a rate of 94 bpm with first degree AV block, the PR interval approximately 300 ms. After a few beats the QRS broadens and the PR interval shortens. Why? Let’s have a close look at the first few seconds to work out exactly what’s happening.
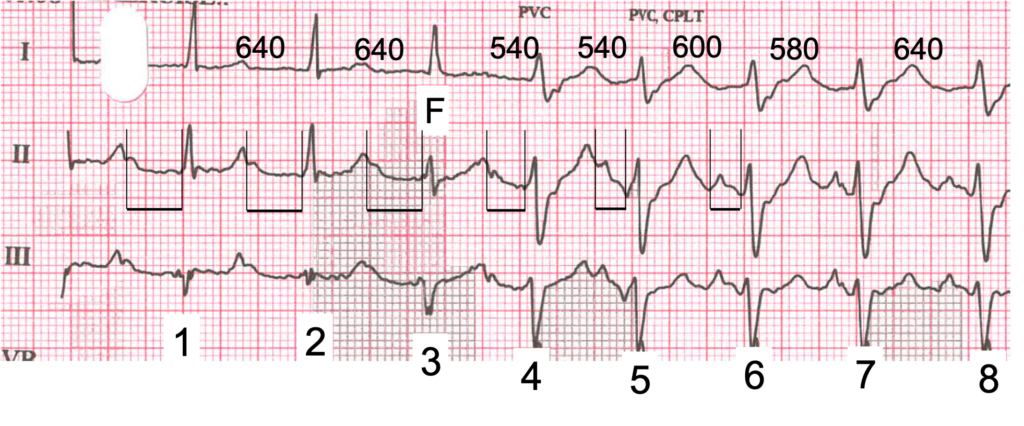
Figure 3. Extract showing the onset of the broad-QRS rhythm. RR intervals are shown in milliseconds; F = fusion.
Beats 1 and 2 in figure 3 show sinus rhythm (RR interval 640 ms) with a long PR interval. Let’s ignore beat 3 for now and go straight to beat 4. The QRS is now broad, the PR interval has shortened considerably and the ventricular rate has increased slightly, the RR interval having shortened to 540 ms. For beat 5 the PR interval has shortened further and the RR interval remains at 540 ms. This is because there is now a VT or accelerated idioventricular rhythm with a rate very close to 100 bpm, and there is AV dissociation – the sinus impulses no longer conduct to the ventricles. It’s not that there is any AV block, it’s just that the ventricular focus discharges before the sinus impulses get the chance to conduct. From beat 6 the ventricular rhythm slows slightly and becomes a little irregular, but even though the sinus node discharge rate is now almost exactly the same as the ventricular rate, there are no conducted beats because the long AV conduction time means that the ventricular rhythm continues to be determined by the ventricular focus discharge rate.
Eventually, the ventricular rhythm stops spontaneously and sinus rhythm with AV conduction resumes. But let’s go back to beat 3: here the QRS is intermediate in shape compared to beat 2, a conducted sinus beat, and beat 4, which is of ventricular origin. This is because beat 3 is a fusion beat: the ventricular focus discharges at exactly the same moment that the sinus impulse reaches the ventricles. This beat alone is very strong evidence that the broad-QRS rhythm that follows is of ventricular origin.
Why can’t this be a supraventricular rhythm with right bundle branch block aberrancy? Because of the shorter and variable PR interval and the fusion beat, indicating AV dissociation, and because there is not a RBBB morphology: the first R wave in V1 is taller than the second, which is the opposite of what is typically seen in RBBB. The QRS morphology and left axis deviation of the broad-QRS rhythm indicate that it probably originates in the left posterior fascicle.
WPW. I think when the axis change there is because of accessory pathway.
Thanks, Anca. I won’t comment on your suggestion just yet. It would be nice to know what other people think. Do others agree with Anca or are there any alternative explanations?
So first impression is that there is extreme 1st degree AV block. However on closer inspection, it appears to be a junctional rhythm with retrograde P waves. QRS morphology then becomes broad and the PR interval appears to be shorter, however, if you map out the p waves (V1 for best view) the rate of the p wave doesn’t actually change, so it’s more likely that the junctional rhythm is now aberrant and the p waves are still retrograde. So possibility maybe that junctional rhythm progressed to a form of AV block causing a broad QRS, or maybe that this is just an accelerated junctional rhythm with intermittent RBBB…?
I really don’t know the answer to this one and I’ve stared at it for quite a while. I’ll attempt to analyse as much as I can, but can’t come to a definitive conclusion.
P wave rate is around 100bpm and is regular throughout the rhythm strip. The P waves are positive in lead II which I assume are sinus P waves, however I cannot see clear P wave polarity in lead I, and P waves in V1 look more peaked than would normally expect.
Ventricular rate is also regular (around 100bpm) aside from slight difference coming in and out of the two QRS morphologies. The narrow QRS with a normal axis has a long PR interval. The wide QRS has a normal (possibly short) PR interval.
Each P wave appears to be related to a QRS complex. I can’t see any obvious AV dissociation or any instances of Wenckebach, flutter etc.
I initially thought that the wide QRS complex was a rate-related right BBB. However, the rate doesn’t actually increase, and the axis is way off – extreme left to northwest axis (also positive complex in aVR), which is not typical for RBBB. It also doesn’t explain the change in PR interval from long to short.
Ruling out other causes of wide complex tachycardia and assuming that each P wave is related to a QRS complex I can only narrow it down to either an atypical BBB or WPW. If it is WPW I honestly don’t think it’s that obvious from the surface ECG (in terms of delta waves and short PR interval).
However, 2 pathways with different conduction properties (i.e. AV node and accessory pathway) would explain the change in PR interval and the northwest axis. So I think Anca might be right unless there some is kind of weird atypical AVNRT that might show these changes. Looking forward to the answer. Thanks for sharing!
I haven’t quite thought it through properly. But I’m wondering whether it’s to do with the bundle branch’s refractoriness- when there’s a delay through the AV node there’s enough time to recover but not when the conduction through the AV is quicker.
Will think more on this though!
Alternating BBB morphology? Looks like incomplete LBBB into a RBBB
A change in the ECG pattern from first-degree AV block to an atypical RBBB pattern with decreased PR interval and increased heart rate can indicate complete heart block from the AV nodal level and the initiation of a facilitated escape beat from a point in the left ventricle.
Thanks, everyone, for taking the time and trouble to have a go at this tricky ECG. I have to say that my explanation – not to be revealed yet – is different from all those advanced so far but because it feels a bit uncomfortable being in a minority of one, I’m going to go back and re-examine the ECG – I may have got it wrong.
In the meantime, a few questions and comments to ponder on in response to points raised so far:
• Why does the PR interval seem to get shorter for the 1st few beats of the broad-QRS rhythm?
• Max says she can’t see any evidence of AV dissociation, but can it be ruled out?
• Pre-excitation has been mentioned but is there anything that looks like a delta wave?
• Does the broad QRS really have a RBBB pattern?
• Arsalan postulates complete heart block, but is it really the case that all the P waves here are blocked when in fact they should conduct? And when the HR is close to 100 bpm, is this likely to be an escape rhythm?
I don’t think this discussion is finished yet! Please keep your comments coming in.
Thanks Dave
In this ECG, we see the beginning and end of a rhythm with a wide QRS. If we accept that the QRS widening must either be of ventricular origin or supraventricular with BBB or an accessory Pathway , then we should be able to find the origin of this rhythm.
I Think morphology of the QRS complex is very important when it comes to distinguishing between supraventricular or ventricular origin of widened QRS complexes.
In my opinion, according to the QRS morphology in lead V1
(R’>R)
This pattern can be considered a ventricular origin with Accelerated Idioventricular Rhythm.
Otherwise, the Ashman phenomenon can be proposed for this ECG.
Looking forward to the answer. Thanks for sharing!
Well spotted – I completely missed that R’>R. Going to give this some more thought!
Thanks Dave
In this ECG, we see the beginning and end of a rhythm with a wide QRS. If we accept that the QRS widening must either be of ventricular origin or supraventricular with BBB or an accessory Pathway , then we should be able to find the origin of this rhythm.
I Think morphology of the QRS complex is very important when it comes to distinguishing between supraventricular or ventricular origin of widened QRS complexes.
In my opinion, according to the QRS morphology in lead V1
(R'<R)
This pattern can be considered a ventricular origin with Accelerated Idioventricular Rhythm.
Otherwise, the Ashman phenomenon can be proposed for this ECG.
Looking forward to the answer. Thanks for sharing!
Thanks Arsalan. You have certainly broadened and extended the discussion. It will be interesting to see what others think, and maybe we will arrive at a consensus.
From Dave and Arsalan’s comments/clues, I’m thinking that the wide complex rhythm might be ventricular. Although at first glance it did look like a RBBB, the abnormal axis and the R being > than the R’ (which I missed) suggests something else. Ashman phenomenon doesn’t make sense to me because the P wave rate is steady throughout. For a P wave to find the right bundle still refractory, surely it would need to arrive earlier than expected? The PR intervals before the narrow QRS complexes are long but they look consistent i.e. first degree AV block. The PR interval before the first wide complex is a bit shorter and then subsequently shorter still (albeit arriving before each wide QRS complex, which to the eye is confusing). I think then this might suggest that a rhythm originating from the ventricle has kicked in before those P waves have had time to traverse the AV node. With a ventricular rate of around 100bpm not sure whether this would be called an accelerated idioventricular rhythm or a VT. That’s all I’ve got Dave!
The PR interval of the first broad complex beat is shorter than the preceding PR, but longer than those that follow; to me this suggests a coincidental timing of a slow ventricular rhythm/tachycardia.
The broad QRS does have a typical RBBB pattern in V6, although the axis favours a left ventricular origin. There is also a little too much variability of the shorter PR, making conduction much less likely.
I really wanted this to be some dual AV nodal pathway related malarkey; next month eh!
Thanks, Max and Scott for some good analysis. Apologies to Scott that there don’t seem to be dual AV nodal pathways – I’m sure they’ll crop up again in the future if people submit some challenging arrhythmias for evaluation. I’ll wait a couple more days, then attempt to provide a full explanation. In the meantime, if anyone has anything else to say – whether in agreement or disagreement with anything that had so far been posted – please submit your comments.