QUESTION
It’s now appropriate to have a more detailed discussion of exactly what may be going on. As I’ve already said, I’m pretty sure that this is atrial tachycardia with Wenckebach block but the Wenckebach sequences are very atypical, with some big, unexpected jumps in the PR interval that have the effect of regularising the ventricular rate so that the ‘dropped beats’ are difficult to see and the Wenckebach sequences are difficult to identify.
Normally in Wenckebach AV block, although the PR interval increases in successive beats, the increases get progressively smaller before the blocked P wave. In this ECG the unexpected jumps in PR intervals in the middle of the Wenckebach sequences can be explained by the presence of dual AV nodal pathways and the switching of conduction from a ‘fast’ to a ‘slow’ pathway. Although we have no direct evidence that this is happening here, we do know that many people have two AV nodal pathways and that the switching of conduction from fast to slow pathway has been documented electrophysiologically in some cases of Wenckebach AV block.
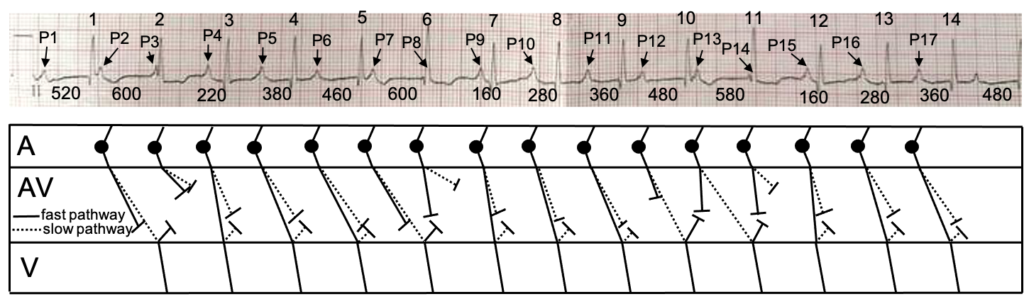
I suspect that Wenckebach periodicity is manifested in both pathways in this ECG and if anyone is interested how I think that both antegrade and retrograde conduction in both pathways may interact to explain the ECG appearances we see, there follows a beat-by-beat analysis of the ECG supported by a laddergram. The laddergram attempts to illustrate impulse conduction through the heart by showing three anatomical tiers – atria, AV node and ventricles – and connecting lines corresponding to the simultaneous ECG above. The big dot shows the origin of the impulses in the atria; in the AV node, conduction in the fast pathway is represented by an unbroken line and conduction in the slow pathway by a dotted line. Conduction always flows from left to right because the horizontal axis of a laddergram represents time, as with the ECG. I have numbered all the QRS complexes and labelled the P waves P1 to P17. All the PR intervals are displayed in milliseconds.
I wish to stress that this is just one explanation and there may be several other plausible hypotheses to explain what we see. There may well be a fatal flaw in my reasoning, in which case I would be grateful if someone would point it out! My thanks go to everyone who has contributed to this discussion, particularly Scott Walton, who continues to keep me on my toes. Further comments are very welcome.
Beat-by-beat analysis:
P2: Conduction is blocked in fast pathway and proceeds down slow pathway to produce QRS 2. The impulse, having got to the bottom of the AV node, both proceeds to the bundle of His and enters the fast pathway retrogradely but is unable to complete its passage back up to the atria because the upper part of the fast pathway is refractory.
P3: Impulse is blocked in both pathways, so there is no QRS.
P4. Conducts rapidly down fast pathway to produce QRS 3. Impulse also enters slow pathway retrogradely but meets antegrade impulse and neither can proceed.
P5: Conducts down fast pathway but more slowly, leading to QRS 4. Slow pathway conduction as for P3 but slower.
P6: As for P5, but conduction is slower. Leads to QRS 5.
P7: Conduction now blocks in fast pathway but is able to proceed in slow pathway to produce QRS 6. This explains the big jump in PR interval. At the bottom of the AV node the impulse enters the fast pathway retrogradely but cannot proceed.
P8: Upper fast pathway has recovered and allows rapid conduction but P8 impulse encounters refractory tissue in the lower pathway from the retrograde conduction of P7 and cannot proceed. Impulse is also blocked in slow pathway, so there is no QRS.
P9: Conducts rapidly via fast pathway to produce QRS 7.
P10: As for P9 but with slower conduction to produce QRS 8.
P11: As for P10, but slower conduction to produce QRS 9.
P12: Impulse blocked in fast pathway, so conducts via slow pathway to produce QRS with a big jump in PR interval.
P13: Impulse conducts some way down fast pathway but encounters refractory tissue due to retrograde conduction of P12 distally and cannot proceed to ventricles. Impulse conducts down slow pathway to produce QRS 11. Impulse also enters lower fast pathway retrogradely.
P14: Impulse conducts down fast pathway initially but encounters refractory tissue for retrograde conduction of P13 and cannot continue to ventricles. Conduction is also blocked in slow pathway, so there is no QRS.
P15: Both pathways mow completely recovered. Conduction as for P9, to produce QRS 12.
P16: As for P10, to produce QRS 13.
P17: As for P11, to produce QRS 14.
Dr Dave Richley,
Associate Lecturer
Newcastle University
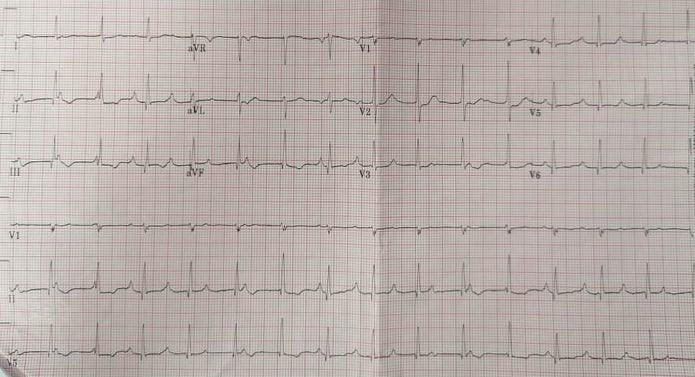
Atrial tachycardia with AV dissociation, narrow QRS, accelerated idioventricular rhythm. ? inferior T wave changes.
Thanks, Stephen. I agree with you that there is an atrial tachycardia – the atrial rate is about 110/min and the P waves have an abnormal shape and axis. You also propose that there is an accelerated idioventricular rhythm but, as you say, the QRS is narrow, and this argues against a ventricular origin. Perhaps, therefore, it is an accelerated junctional rhythm but if so, why would there be AV dissociation? Wouldn’t we expect some of the P waves to conduct to the ventricles? Also, wouldn’t it seem unlikely that we have 2 different, independent simultaneous rhythms – an atrial tachycardia and an accelerated junctional (or idioventricular) rhythm?
There appears to be a lengthening of the PR interval.
It could be atrial tachycardia with wenckebach.
Interesting suggestion, Mary! Does anyone agree, or disagree? Or do most people just find this one unfathomable? If this is Wenckebach block, it’s an atypical form because there is no obvious pause. Is there any possible explanation for this?
3rd degree AV block with a supraventricular (narrow QRS) escape rhythm probably from within the bundle of His
Thanks, Julian. Complete AV block would certainly explain the apparent AV dissociation, but can we be sure that there really is AV dissociation here? And, can we really describe this as an escape rhythm when the ventricular rate is just under 100/min?
The RVH pattern suggests this is a paediatric ECG, so an ‘escape’ rate close to 100bpm at rest is plausible.
No discernible AV or VA conduction, with stable/regular A and V rates.
P-waves are positive in inferior leads, which is a normal axis, so possible congenital CHB with accelerated junctional ‘escape’, or simply AV dissociation.
I’d love this to be the old transplant with native RA left intact chestnut, but I really can’t find any P-waves other than the peaky ones.
Good ECG
Thanks, Scott. the person who sent me the ECG is a consultant in adult cardiology so I don’t think this is a paediatric case.
Although it appears to have a ‘regular’ R – R, could it be Atrial Tachy with Wenckebach ?
Good question!
Could it be a wandering atrial pacemaker?
Thanks, Helen. For that to be the case there would have to variable P wave morphology and variable atrial rate. I don’t think we are seeing that. Also, this wouldn’t explain the marked variation in PR interval.
I see you annotated the second half of the ECG which fits the provided “answer”, whereas the 3rd R-wave of the complete ECG which has the “return to normal” PR interval is not 160ms, therefore this interpretation does not explain the entire presented ECG.
You’re such a cynic, Scott! It’s quite common for Wenckebach sequences to vary in their length, conduction ratios and PR intervals, but I have prepared a detailed description including laddergram, to explain what I think may be happening throughout the entire ECG. It’s a bit complicated and it may be wrong so I’ll hang on a few days before posting it to see if anyone else wishes to add anything first. Are you sticking with your original explanation?
Diplomatic choice of words; I think my cynicism increases with how atypical things are, although typical presentations wouldn’t be quite as interesting. Whether it’s common for the first PR of each WKB sequence to vary is debatable (reference please – it’s not in Mobitz’s original definition), unless it’s vagally mediated or infra-nodal block.
Just like CHB masquerading as 2:1 AVB during coincidental A and V rates – a longer recording would yield the truth, and hopefully display the PR interval which is too short to be conducted and confirms dissociation (or doesn’t!).
To be fair, I’ll have to admit that it’s not common for the first PR interval of each Wenckebach sequence to vary – I think my ECG collection is probably bit unrepresentative of normality and has biassed my thinking. Nevertheless, such variation does exist and it’s usually seen when there are other atypical features of the Wenckebach sequences. I’ll try to post my full explanation tomorrow. Of course, it may be wrong and if you think it is, I would very much welcome any further opinions or ideas that you have.
By looking at the ECG without reading all the rest my first thought was AV dissociation. Atrial rate is higher than ventricular rate but not too different almost equal. Could it be Isorhythmic AV dissociation?
I agree that it looks at first sight as if there is AV dissociation, but have a read of my full explanation and see what you think.