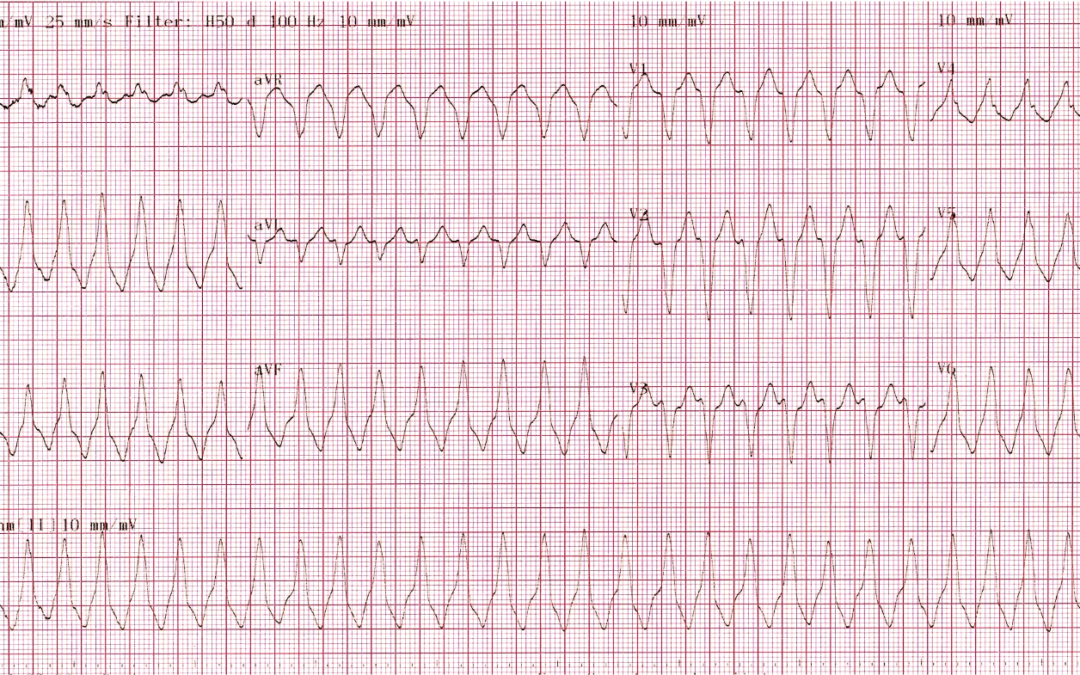
This ECG was recorded from a 32-year old male while he was experiencing ‘palpitations’. He had no history or signs of heart disease and when he was back in sinus rhythm he had an echocardiogram which was entirely normal.
What is the rhythm most likely to be?
Answer
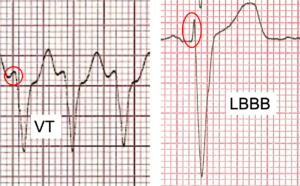
Figure 1. Initial QRS deflection (ringed in red) contrasted in VT and LBBB.
As we have previously discussed, any regular, broad QRS tachycardia should be considered VT unless it can be proved otherwise. So, is there anything about this ECG that leads us to think that it is likely to be an aberrantly conducted SVT? A P-wave preceding every QRS would certainly lead us in that direction, but we don’t see that here. An absolutely typical bundle branch block pattern might be strong evidence for an SVT with aberrant conduction, and the QRS morphology here is certainly similar to that seen in left bundle branch block(LBBB), but is it typical? When the QRS is broadened as a result of a fixed bundle branch block (left or right) or because of rate-related aberrancy, the QRS usually has an initial sharp deflection before the complex broadens out. This is because the electrical impulse that enters the ventricles proceeds rapidly at first before encountering the tissue that is not able to conduct, at which point impulse propagation continues more slowly. This is in contrast to the situation with a beat of ventricular origin, as in ventricular tachycardia. Here the impulse proceeds slowly from the moment it emerges fromthe ventricular muscle, so the QRS is broad from the start. Often in this case the QRS finishes more quickly than in started because the wave of depolarisation within the ventricular muscle may encounter healthy conduction tissue which enables it to speed up.
The easiest way to assess the initial QRS deflection is to examine a biphasic complex – one with both a negative and a positive component. Figure 1 contrasts the QRS of the ECG under discussion with one from someone with LBBB. Both extracts are from V3. The QRS on the left begins with a slow-rising deflection (ringed in red), and this is because the rhythm is VT. This is very different from the initial QRS deflection (again ringed in red) in the complex on the right, which is very sharply inscribed because this is a case of LBBB. So, although the QRS morphology in this tachycardia resembles that of LBBB, it is not absolutely typical of it.
Why should an otherwise healthy 32-year old suffer from VT? This is almost certainly an idiopathic VT, the group of VTs that have in common that they are not due to structural heart disease or any metabolic, electrolyte or drug-induced disorder. In October 2021 we discussed the subject of idiopathic VT and the example I showed then was of a fascicular VT. However, the most common type of VT is right ventricular outflow tract (RVOT) tachycardia, a VT that originates, as the name implies, in the outflow tract of the right ventricle. The characteristic ECG features of this tachycardia are a left bundle branch block QRS morphology and an inferior QRS axis (positive complexes in leads II, III and aVF).
This then is almost certainly a VT and in view of the history and ECG features, it is most likely to be an RVOT VT. RVOT VTs can often be terminated acutely by a vagal manoeuvre or by the administration of adenosine or verapamil. They arerarely lethal, but if troublesome they can often be cured permanently by catheter ablation of the site of origin of the VT.
For anyone interested in more detail of how the width of the initial (and terminal) portion of the QRS can be used to help differentiate between VT and SVT with aberrancy, the description of the diagnostic algorithm proposed by Vereckeiet al in 2007 may be helpful (1).
1. Vereckei A, Duray G, Szénási G, Altemose GT, Miller JM. Application of a new algorithm in the differential diagnosis of wide QRS complex tachycardia. Eur Heart J. 2007 Mar;28(5):589–600. DOI: 10.1093/eurheartj/ehl473
AVRT given the history. In V4 I can convince myself that there are regular (?retrograde) P waves.
I assume to make it not too obvious you left out the fact that the sinus ECG would likely have features of WPW?
Thanks for your comments, Jon. I think the deflections in V4 that you think may be retrograde P waves are actually part of the QRS. AVRT has to be considered a possibility in a case like this but why is the QRS broad? Is it because of LBBB aberrancy or because the AVRT is antidromic? In my experience the QRS in antidromic AVRT is usually broader and more bizarre than here, but I admit that my experience is limited. Or is there another, very different and possibly more likely, explanation?
Firstly could be VT until otherwise proven. Steps I would take in this analysis:
No evidence of AV dissociation with no fusion beats. Not extreme axis deviation. Precordial leads do not have either complete positive or negative concordance. It is essentially LBBB morphology. RS interval appears <100ms I believe.
For the argument of SVT with LBBB aberrancy. Structurally normal heart. No Past cardiac Hx. Unlikely to be VT.
Could it be as simple as AVNRT with LBBB morphology?
Thanks for your analysis, James. You rightly suggest that the rhythm should be considered as VT unless proven otherwise and you list some of the characteristics that are commonly associated with VT rather than SVT with aberrancy, and you correctly note that none of these characteristics are present. The big question is: does the absence of any of the ECG features typically associated with VT prove that the rhythm is SVT? Or do we need more positive proof of SVT before we diagnose it? Another question: in this case does the QRS complex have a typical LBBB morphology, or is there something definitely atypical about it? These questions are not easy!
Deep inferior axis and pseudo-LBBB QRS morphology. I can’t discern any atrial activity, independent or otherwise, which may suggest AVRT/AVNRT, but my money would be on RVOTVT despite the relatively mild symptoms given a rate approaching 190bpm.
Having just done a patient case study on WPW, I’m wondering if is this antidromic AVRT?
Given his age, structurally normal heart and the fact it appears he was not syncopal, VT seems unlikely.
There are also negative complexes in V1-3, but positive complexes V4-6. Doesn’t this make AVRT more likely than VT?
Thanks, Adi. Antidromic AVRT certainly has to be considered in a case like this but is the QRS morphology really typical? Is there anything else that should be given serious consideration?
I may being far too simplistic here as I can’t zoom in and look for rogue P waves. But monomorphic VT ? In an otherwise normal looking heart (on echo)
Thanks, Debbie. There’s nothing simplistic about assuming that a regular, broad QRS tachycardia is VT. Many would argue that this is the correct approach to take!
RVOT? Positive inferior leads. LBBB pattern through chest leads. Looks like a VT with the rate being around 220bpm.
RVOT VT would be my suggestion, LBBB morphology in V1 with inferior axis in a relatively young patient with no structural heart disease. First beat could potentially be a fusion beat at the onset of tachycardia as slightly different morphology from the rest.
Based on the broad QRS with a LBBB configuration and the structurally normal heart (as well as the fact the patient is haemodynamically stable) I would lean towards RVOT VT.
I think the large positive inferior complexes, precordial transition, normal echo and young stable patient seem suggestive of an idiopathic RVOT VT
Thanks for all the recent contributions to the discussion. A new consensus seems to be emerging. Scott, Emma, Leah and Katie and Esther all suggest that this may be RVOT VT. Do others agree or disagree? I’ll offer my thoughts within the next day or two.