Something a bit different this month: two 3-lead extracts (A and B) from an ambulatory ECG recording. I have numbered the beats in each strip to facilitate discussion. I’m afraid I don’t have any clinical details but my question is a simple one: what on earth is going on here?
The answer
I have drawn laddergrams to illustrate what I think is probably happening in these two Holter extracts. Let’s deal with the two strips individually.
In strip A (figure A) there is a fairly regular atrial rate at about 80 bpm with alternating normal/long PR intervals, producing an irregular ventricular rhythm with coupled beats. What could be the cause of the alternating PR intervals? As several people have reasoned, this phenomenon is likely to be due to dual AV nodal pathways – one fast, the other slow.
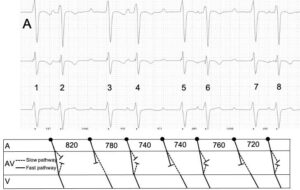
When there are dual AN nodal pathways, though, the PR interval is usually constant because the sinus impulse always reaches the ventricles via the fast pathway. So, I think that in this case there must be 2:1 block in the fast pathway, which allows the sinus impulse to reach the ventricles via the slow pathway in alternate beats. Let’s look at this more closely in figure A. Beat 2 has a normal PR interval because the sinus impulse travels down the fast AV nodal pathway (shown by the unbroken line in the AV nodal tier of the laddergram) to the ventricles. The impulse also enters the slow pathway (shown by the dotted line) at the same time as it enters the fast one but is not able to proceed to the ventricles by this route. This is because once the impulse has reached the far end of the fast pathway it enters the slow pathway retrogradely where it meets the slowly-progressing antegrade impulse; the two impulses meet head-on and extinguish each other. Moving on to beat 3, the sinus impulse again enters both AV nodal pathways simultaneously but this time, probably because of disease, the impulse is unable to proceed down the fast pathway. It therefore conducts down the slow pathway to produce a beat with a long PR interval. When we get to beat 4, the fast pathway has had long enough to recover completely and it therefore conducts with a normal PR interval again, and this simple sequence keeps repeating.
Moving on to strip B (figure shown below), we can see that here there are 2 non-conducted P waves, and this is likely due to intermittent block in the slow pathway as well as 2:1 block in the fast pathway. Beat 2 is conducted with a normal PR interval because of conduction down the fast pathway. As in similar beats in strip A, the slow pathway fails to conduct not because of ‘block’ but because the impulse, having travelled down the fast pathway, enters the slow pathway retrogradely and stops the antegrade impulse in that pathway from progressing any further.
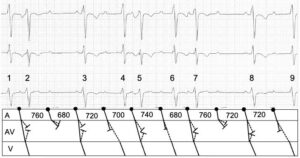
After beat 2 there is a P wave not followed by a QRS and presumably this is due to simultaneous block in both pathways, providing evidence that it is not only the fast pathway that is diseased – there must be disease in the slow pathway too. For beat 3, both pathways have had time to recover and the ventricles are activated via the fast pathway, as for beat 2. Beat 4 has a long PR interval because the 2:1 block in the fast pathway continues and activation of the ventricles is brought about by transmission down the slow pathway. Beats 5, 6 and 7 continue this pattern of 2:1 block in the fast pathway, although beat 6 has a slightly shorter PR interval than might be expected and I don’t know why. After beat 7 there is another blocked P wave, presumably because of simultaneous block in both AV nodal pathways. Beats 8 and 9 continue the short PR/long PR sequence. Thus, it appears that in ECG B there is 2:1 block in the fast AV nodal pathway and occasional block in the slow pathway. Wenckebach AV block is almost always due to a conduction disorder within the AV node, so in this case the intermittent block in the slow pathway may well be due to the Wenckebach phenomenon. I did wonder whether some of the variation in conduction might be due to changes in the atrial rate but on examining the PP intervals I can’t see any evidence of this.
In summary, this ECG appears to show evidence of dual AV nodal pathways with 2:1 block in the fast pathway and intermittent Wenckebach block in the slow pathway, producing second-degree AV block in strip B. If you have an alternative theory or can provide any additional explanatory detail, please post your comments.

Sinus rhythm with dual AV nodal pathways, then in strip B we have 2nd degree AV block of the slow pathway. I’m not sure why complex B6 has a shorter PR interval though.
Thanks, Scott. Could you add a bit more detail, eg explaining the alternating PR intervals in strip A? Normally, with dual AV nodal pathways conduction always proceeds down the fast one and the PR is constant. Like you, I am also not sure why complex B6 has a shorter-than-expected PR interval.
A laddergram would be better than words, however, simultaneous anterograde conduction via both limbs; conduction of the slow pathway enters the distal portion of the fast pathway retrogradely, depolarising it and so leaving it refractory for the next sinus P-wave, therefore conduction takes place via the slow pathway which has had adequate recovery time, on alternating cycles.
Would be interesting to see any strips where the P-P interval is a little longer, outside of the refractory period of the fast pathway. To see if we have any sustained conduction down the fast pathway before it conducts down the slow.
Not sure I completely follow your explanation but, as you say, a laddergram often explains things more clearly than words, so I’ll post a couple of ladder grams in a few days’ time to illustrate what I think may be going on, and maybe you could let me know what you think? In the meantime, it would be nice to know if anyone else has any ideas.
Just to add, what we therefore see in strip B as overt AV-block is likely the result of both limbs being refractory when the sinus P-wave arrives, due to the increased atrial rate; many presentations of AV and BB blocks are actually the result of excessively long refractory periods rather than an inability to actually conduct.
You make a very good point about AV blocks and refractory periods. AV block is often not fixed, but dependent on atrial rate.
Rhythm-wise, it looks to me like sinus rhythm with first degree AV block (long PR interval) with supraventricular bigeminy.
Ignore previous comment. I was only looking at A! B has thrown me.
Yes, it’s not straightforward is it?!
My guess (out of the box), complete AV nodal block with two pacemakers originating under the block (there is of course still some BBB present as the QRS aren’t exactly the most narrow).
Thanks, AM. If this is complete AV nodal block, then there should be complete AV dissociation, but in strip A there seem to be alternating PR intervals. Also, if there are 2 different foci producing escape beats, why does one of them discharge after an RR interval of only about 500 ms? This is a bit short for an escape beat!
I think I agree with Scott, strip A jumped out at me as an example of dual AV nodal physiology. Strip B needed some thinking about but if you think of the conducted beats as being the short coupled ones from strip A then both pathways being refractory (block of the slow pathway) is likely. I know you say there is no patient history available but it would be helpful to know if they’ve had a previous AVNRT ablation that may have partly recovered
Thanks, Katie. I’m sorry but I really don’t know anything about the patient. Many people have been kind enough to share Interesting ECGs with me over the years but they often don’t pass on to me – probably because they don’t know – any history. I know it can be a bit frustrating, but with arrhythmias I think it’s still useful and interesting to try to work out what is happening.
A good proposed model Dave, nice work, the two assumptions being AV block in the fast pathway, and a separate block in the slow pathway.
My proposed model was based on slow retrograde conduction of the fast pathway and a prolonged recovery time of the slow pathway. Either way, overt second degree AV block with a broad QRS mandates pacing in most patients, particularly older people with relevant symptoms/history.
We may have to consider B6 as a coincidental junctional extrasystole, that failed to alter the surrounding rhythm due to it’s minimal prematurity, for want of a better explanation.
It’s probably worth adding that in the context of intraventricular conduction delay (as in this example), block is more likely to be Hisian, or infra-Hisian, rather than AV nodal, although of course concurrent independent blocks of both are possible.
Evidence of dual AV nodal pathway physiology can be observed more often than we probably realise, and is almost always displayed by the PR intervals preceding and following interpolated ventricular extrasystoles, we simply choose not to think about it.
Thanks, Scott. We’ll never be sure exactly what’s going on here, but to quote the legendary arrhythmia expert, the late Dr Mauricio Rosenbaum: “Every complex arrhythmia has at least 3 different explanations!”. I agree that dual AV nodal pathways are much more common than is generally appreciated and this is a subject I may return to in the future.