Last month’s ECG was quite simple, so to make up for it this month’s is perhaps a bit tricky. Once again, it’s the rhythm I’m interested in, so what exactly is going on? Any answer should account for the ventricular irregularity and the relationship, if any, between P waves and QRS complexes.
Answer
First of all, this is not THE answer, it is AN answer. Despite much examination and analysis, and the comments of others, I’m still not sure what is going on here. I have modified my original explanation as a result of comments posted by Scott Walton and Arron P, and private exchanges also with Arron.
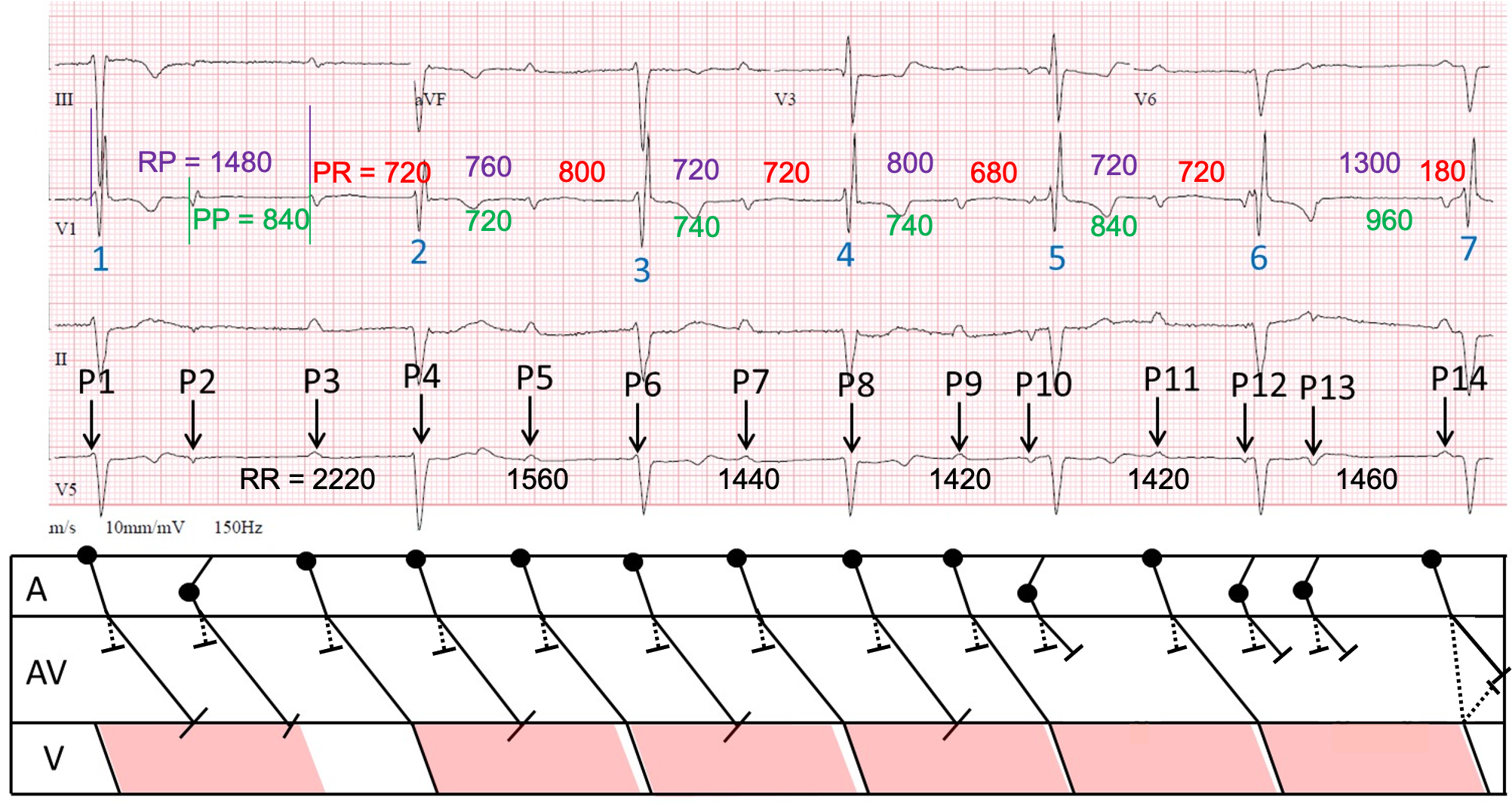
I have constructed a laddergram, on which I have displayed my measurements of the RR intervals (black), some PP intervals (green) and RP intervals (purple), in the hope (probably forlorn) that they might reveal some sort of pattern. I propose that there are dual AV nodal pathways and I have represented the fast pathway conduction with a dotted line, and the slow pathway conduction with an unbroken line. I have shown what I postulate may be the refractory period of the ventricular tissue with a pink parallelogram.
First, the basics. There is sinus rhythm with an atrial rate of about 80 bpm. There is also left anterior fascicular block and right bundle branch block, slight ST depression in I, II and aVL, with slight ST elevation in II and aVR. Additionally, there are very small Q waves in V2 and V3, with very small initial R waves, and dominant S waves, from V4 to V6. The T waves are inverted in V4 and V5.
But let’s concentrate on the rhythm and atrioventricular conduction, which are not straightforward. I think that what we may be seeing is basically sinus rhythm with 2:1 AV block and long PR intervals, complicated by non-conducted atrial premature beats (APBs). The RBBB and LAFB tell us that there is disease of the bundle branch system; the long PR intervals suggest that there is concomitant AV nodal disease and it is difficult to be sure at what level the problem lies when atrial impulses fail to conduct at all.
I’ll go through the ECG beat by beat, explaining what I think may be happening, but then admit the weaknesses in my theory and consider an alternative hypothesis.
It’s difficult to say much about QRS1 because we can’t see enough of what precedes it.
P1, visible only as a small defection merging with the start of QRS1, is a sinus impulse that fails to conduct because it arrives at the ventricles when they still in their refractory state. P2 is an APB and also fails to propagate to the ventricles. P3-P9 are all sinus impulses. P3 is able to conduct to the ventricles and is therefore followed by QRS2. P4, which is almost completely masked by QRS2, arrives at the ventricles while they are refractory and therefore does not elicit a QRS. P5 does conduct all the way to the ventricles and results in QRS3. P6, visible as a small deflection merging with the start of QRS3, is blocked because the ventricles have had insufficient recovery time. P7 succeeds in conducting, producing QRS4. P8 is blocked, but P9 conducts and results in QRS5. P10 is an APB, which blocks in the AV node and although QRS5 follows P10, there is no connection between the two events. P11, another sinus impulse, conducts, resulting in QRS6. P12 and P13 are both APBs, and they fail to conduct through the AV node. P14, the final sinus impulse, conducts with a normal PR interval, resulting in QRS 7.
Why should P14 conduct with a normal PR interval when all the other sinus impulses that manage to conduct do so with a very prolonged PR interval? I think the answer is provided by the preceding PP interval of 960 ms, which is the longest on the ECG. So far in this ECG the fast AV nodal pathway has not been able to conduct because the atrial rate is too fast: its refractory period is just too long, so the sinus impulses conduct instead down the slow pathway, hence the long PR interval. But after a PP interval of 960 ms the fast pathway is able to conduct, as suggested by Scott, and the impulse whizzes down to the ventricles. When it reaches the bottom of the AV node it starts to conduct retrogradely up the slow pathway, where it meets the impulse travelling down it and the impulses block each other.
The main weakness of this explanation is that the PR intervals of what I assume are conducted beats are not constant: they vary between 680 and 800 ms. If there is 2:1 block, the PR intervals should be constant. PR intervals can vary as a result of a changing atrial rate: shorter PP intervals are sometimes followed by longer PR intervals, but I don’t see evidence of this here. Perhaps there are other factors at play which I have not been able to identify.
Arron P’s alternative explanation is that this is essentially high-grade AV block with a junctional escape rhythm and one conducted beat, which results in QRS2. This would explain the varying PR intervals, because if the explanation is correct there is AV dissociation for most of the ECG. However, if the blocking of P2 creates a pause which allows P3 to conduct to the ventricles, it is not clear to me why other sinus impulses, eg P11, do not succeed in conducting also. It is also not clear why a junctional escape beat does not intervene before QRS2, since the RR interval to QRS2 is by far the longest on the ECG. Also, although most of the remaining RR intervals are pretty constant at 1420-1460 ms, supporting the concept of an escape rhythm, the 2nd RR interval is significantly longer at 1560 ms, which argues against it.
So, I’m still not sure what is going on and would welcome further opinions.
This is my last ‘ECG of the Month’, because I have finally run out of suitable material. Thanks to everyone who has contributed to this feature over the last 2 or 3 years. Most of the ECGs have been challenging to interpret – that was the intention! – but I hope that some people have learnt something from some of the discussions: I certainly have.
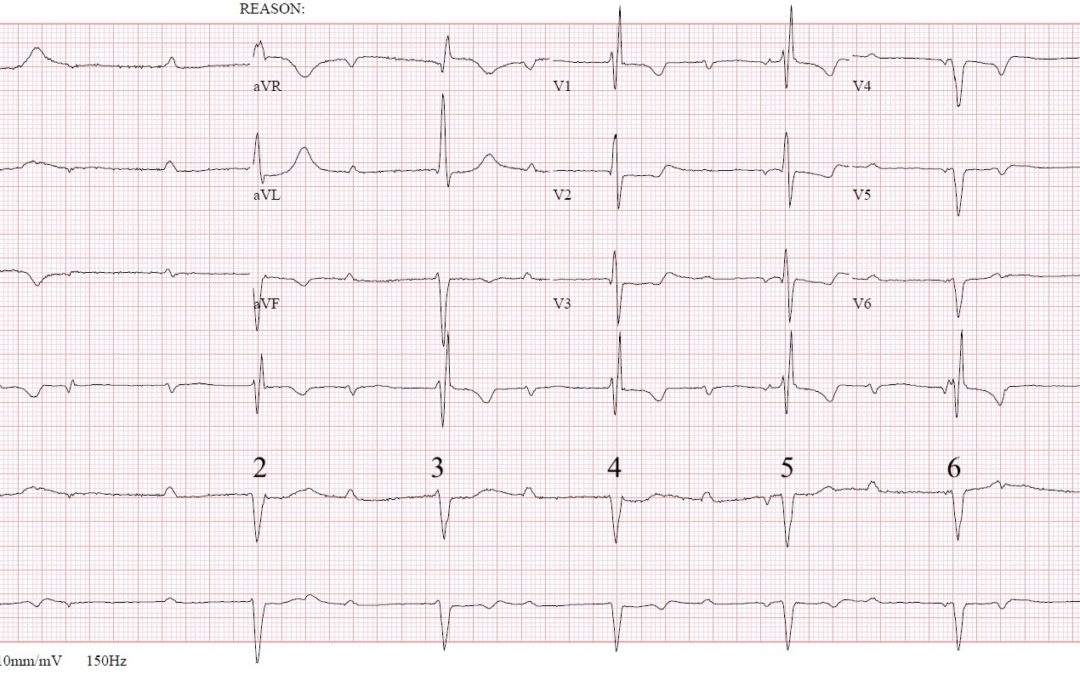
CHB. BFB with RBBB & LAFB. Initial pause- no escape beat occurred. Poor R-wave progression. STD I & aVL. Nonspecific STT changes several other leads. Pacing occurring from around Lt Posterior Fascicle. Will need pacemaker placement (urgency depending on symptoms, hemodynamics, etc.).
Thanks very much for your suggestions, Marc. You interpret this as CHB, so presumably you believe that there is complete AV dissociation, but I wonder if this is definitely the case? Also, you say that there is RBBB + LAFB, but if, as you suggest, there is a left posterior fascicular escape rhythm then perhaps it is inappropriate to invoke RBBB + LAFB as an explanation for the QRS morphology.
Sinus rhythm long pr inverted p wave. Some lead pr variable. I suspected this is a case sinus bradycardia interrupted by atrial echo beat follow by junctional escape rhythm. Most likely this echo beat involved dual pathway. Another thought is escape echo bijeminy although question is long pr but i suspected it is also plausible this long pr.may be this conceal his extrasystole cause psudo av block. Any previous rheumatic heart disease? Your master opinion needed sir.
Thanks for your comments. I’m not sure what is going on here but I’ll reveal what I think may be happening in about a week’s time.
Underlying rhythm is sinus, with trifascicular block – LAD, BBB & marked first degree AV block. I’m not convinced it is CHB as PR intervals are almost regular until beat 7. I think there is some non-conducted atrial ectopy involved, certainly followed beat 1 & 6. Not sure about the odd Pwaves proceeding 5 & 6 ? Ectopy too. Beat 7 could be junctional or deterioration of AV block. I’m sure there’s a much more technical way of saying all that, but that what I take from it at first glance
Some great observations there, Daisy, but I don’t think that everything is explained just yet. For instance, if beat 7 is a conducted beat, why does it have a much shorter PR interval than the other beats? If it is a junctional escape beat, why aren’t there other junctional escapes after the same RR interval? I think there is a subtle but important detail that has not yet been detected and that may provide the key to explaining the arrhythmia in full.
This is a cracking ECG with very interesting oddness. The QRS morphology has already been extensively described above.
The PR interval of beats 2 to 6 suggests sinus bradycardia with a marked first degree of ~700ms (so I think I agree with Daisy).
There are also the ectopic P-waves (preceding beats 5 and 6, and another following beat 6).
The atrial ectopic falling just before beat 5 fails to interrupt the sinus interval – which if recall correctly could represent sinoatrial entrance block.
The initial longer RR interval is caused by an atrial ectopic which does reset the SA node in the usual fashion, but fails to AV conduct, whilst the atrial ectopic P-wave following beat 6 possibly conducts super slowly (PR 1,000ms) – it’s unlikely to be an escape beat or beat 2 would have done the same.
I very much look forward to the exceedingly complex laddergram.
I always enjoy reading your comments, Scott, and l think that you have gone a long way to explaining this arrhythmia but that you are missing something of importance. Unless, of course, I’m seeing something that isn’t there! If the atrial premature beat after beat 1 re-sets the sinus node and if there is an underlying sinus bradycardia, as you suggest, why does the next sinus P wave – before beat 2 – appear after a much shorter PP interval than normal? You’re right to assume that I’ve done a laddergram but I don’t think it’s exceedingly complicated and I look forward to posting it in due course.
I shouldn’t have been so quick to disregard the QRS morphology, so I missed the subtle variability of it, which I think represents an additional sinus P-wave, making this marked 1st degree with concurrent 2:1 AV block, and atrial ectopy that interrupts the sinus rate in a normal way, and is mostly nonconducted.
Beat 7 is still a bit odd, but I’m sticking to very long conduction from the second of two consecutive atrial ectopics.
Good observation, Scott. I’m not sure I agree with you about beat 7 but I’ll re-assess my original assumption and see if your explanation makes more sense than my, so far undisclosed, theory.
Beat 7 could be anterograde conduction via the fast AV pathway, which is apparently blocked/perpetually refractory elsewhere, as it has been given plenty of recovery time from two blocked ectopic P-waves.
There is an underlying sinus rhythm at around 79 bpm (some P waves are hidden in the QRS complexes seen as small intermittent R waves). There is also several non-conducted premature atrial ectopics.
I believe there is a high level of AV block and that beat 2 IS conducted. This is then followed by an escape rhythm at 42 bpm causing AV dissociation. I think the escape rhythm may be junctional in origin rather than ventricular despite Q waves V4 – V6 (perhaps RBBB + LAFB + old MI).
The first atrial ectopic causes concealed conduction of the AV node but is blocked from capturing the ventricles. This pause gives chance for the next sinus P wave to conduct because the AV node has recovered. No further beats conduct due to the escape rhythm (the AV node is still refractory or blocked when the P waves appear). The only reason we have a single conducted beat is due to timing of that first atrial ectopic. It allows the AV node a longer time to recover to allow conduction.
I believe there is concealed conduction because I would have expected the escape rhythm to appear as soon as there was a pause longer than 1560ms (as that’s the time in which is starts after beat 2).
I am hoping you agree with my thought process Dave, looking forward to your explanation.
I have drawn a brief laddergram to help illustrate my thoughts however I am unable to post pictures here.
Thanks very much for this, Arron. I agree with you about the underlying sinus rhythm but I’m not convinced that there is an escape rhythm. However, I may be wrong so I would be grateful if you would send me your laddergram so that I can re-assess my explanation. Yours may make more sense.
Has there been some kind of surgical intervention in the past?
I’m sorry, I don’t know.